Tobacco Control
Giving What We Can no longer conducts our own research into charities and cause areas. Instead, we're relying on the work of organisations including J-PAL, GiveWell, and the Open Philanthropy Project, which are in a better position to provide more comprehensive research coverage.
These research reports represent our thinking as of late 2016, and much of the information will be relevant for making decisions about how to donate as effectively as possible. However we are not updating them and the information may therefore be out of date.
Cause Area: Tobacco Control
Tobacco kills up to half of all people who use it (i.e. shortens their lifespan), and has a global death toll of almost 6 million people per year (600,000 of whom are non-smokers exposed to secondhand smoke).12 This figure is expected to rise to 10 million deaths per year by the middle of this century.3 In response to these figures and the detrimental effect of tobacco use, the tobacco control policies and anti-smoking mass media campaigns conducted in developed nations have resulted in decreases in incidence of lung cancer and other common diseases.4 Meanwhile, however, many developing countries have not had the benefit of these policies or campaigns and, as a result, deaths due to smoking-related diseases are increasing (see Figure 11).5678
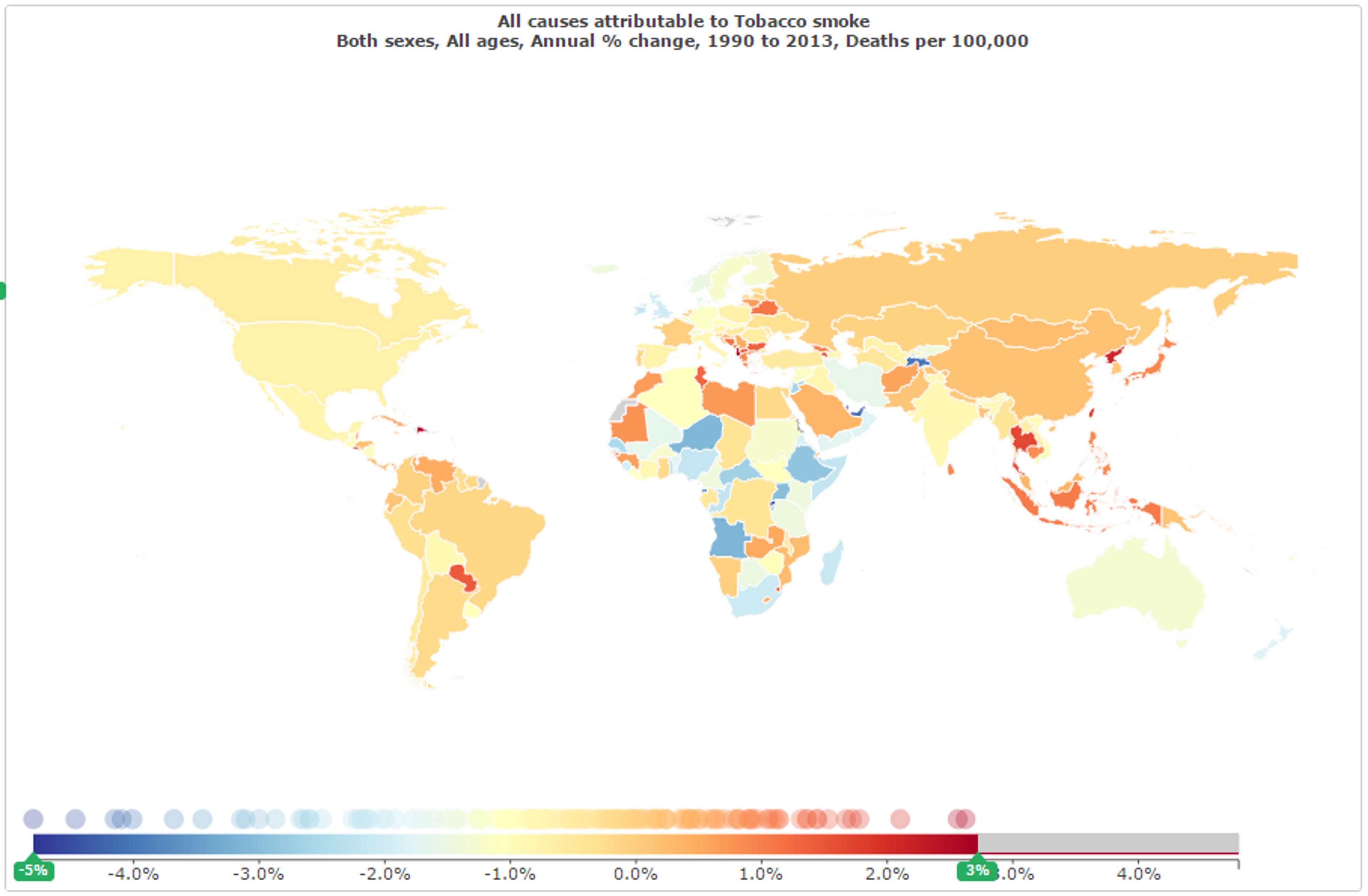
Figure 11: Rate of change of deaths attributed to tobacco smoke between 1990 and 2013;9
The total health burden is also particularly large in developing countries. Due to the uneven distribution of population between developed and developing nations, a large proportion of total deaths due to tobacco use occur in nations such as India and China (see Figure 12). While tobacco and related diseases such as lung cancer may constitute a greater proportion of deaths in developed nations, the absolute number of deaths in nations still in the process of developing provides a problem of greater scale, and hence of potentially much greater impact. Due to the generally lower cost of interventions and neglectedness of public health in these nations, a greater impact can be achieved by improving awareness of and controls on tobacco in these countries than by doing so elsewhere (see Sections 2, 3, and 6 below).
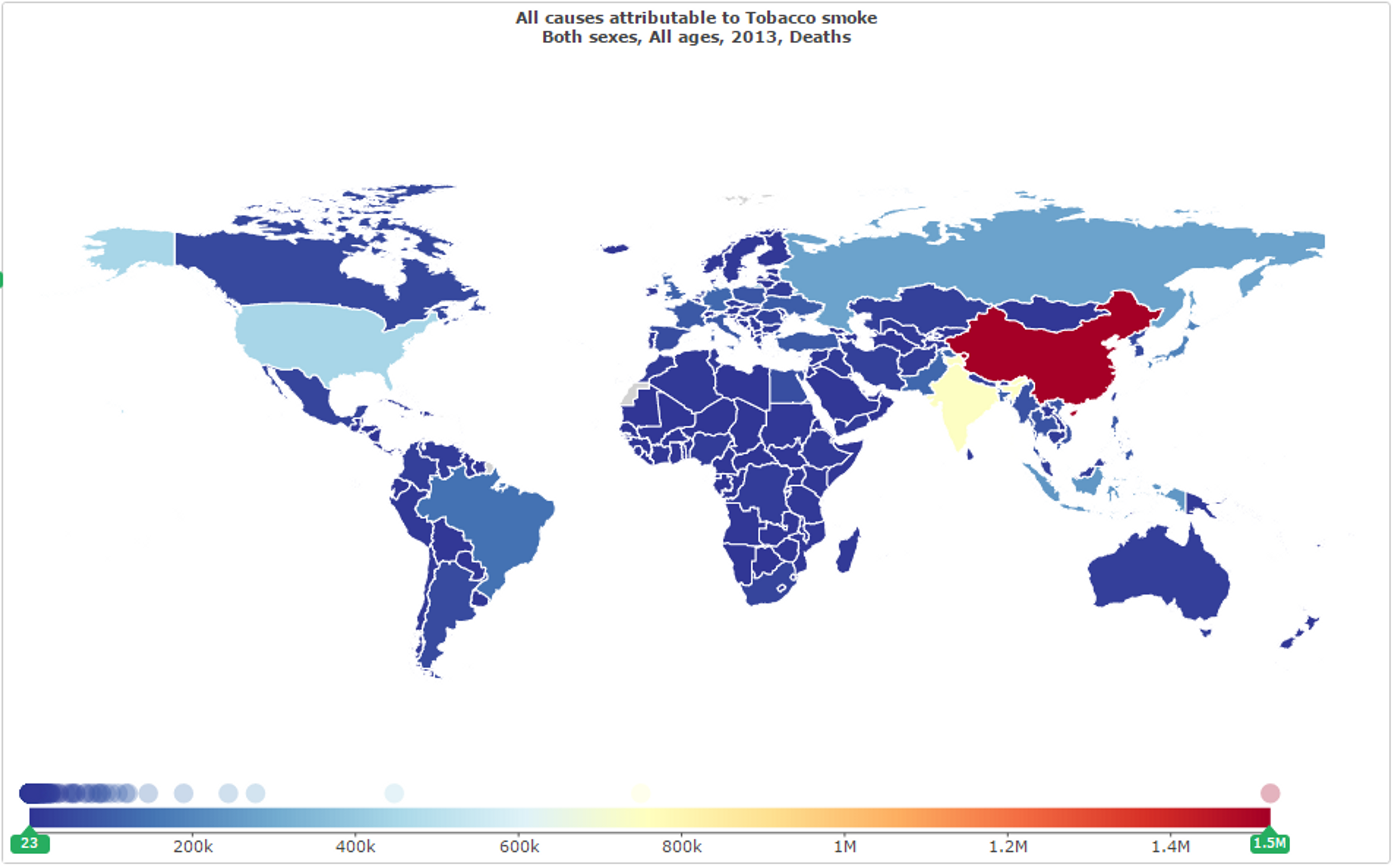
Figure 12: Total deaths attributed to tobacco smoke by country in 2013;10
In developing countries more widely, tobacco use accounts for 9.92% of all deaths (and 4.9% of DALYs incurred), as shown below in Figure 13, which is a greater proportion than all deaths from malaria (2.05%), from HIV (3.1%), from nutritional deficiencies (1.56%), or even from all physical injuries (9.5%).11 These deaths due to tobacco are largely made up of cancer deaths (1.63% of all deaths in developing countries and 16.39% of deaths due to tobacco smoke)12 but also includes various other diseases for which tobacco use increases incidences or chance of death - among them, ischemic heart disease, stroke, hypertensive heart disease, diabetes, chronic obstructive pulmonary disease, asthma, lower respiratory infections, and tuberculosis. Similarly for DALYs incurred by tobacco use, 14.73% are due to cancer (0.72% of all DALYs incurred), but tobacco also makes large contributions to those many other conditions.13 Interventions which reduce tobacco use hence have the potential to reduce the burden of a wide range of diseases.
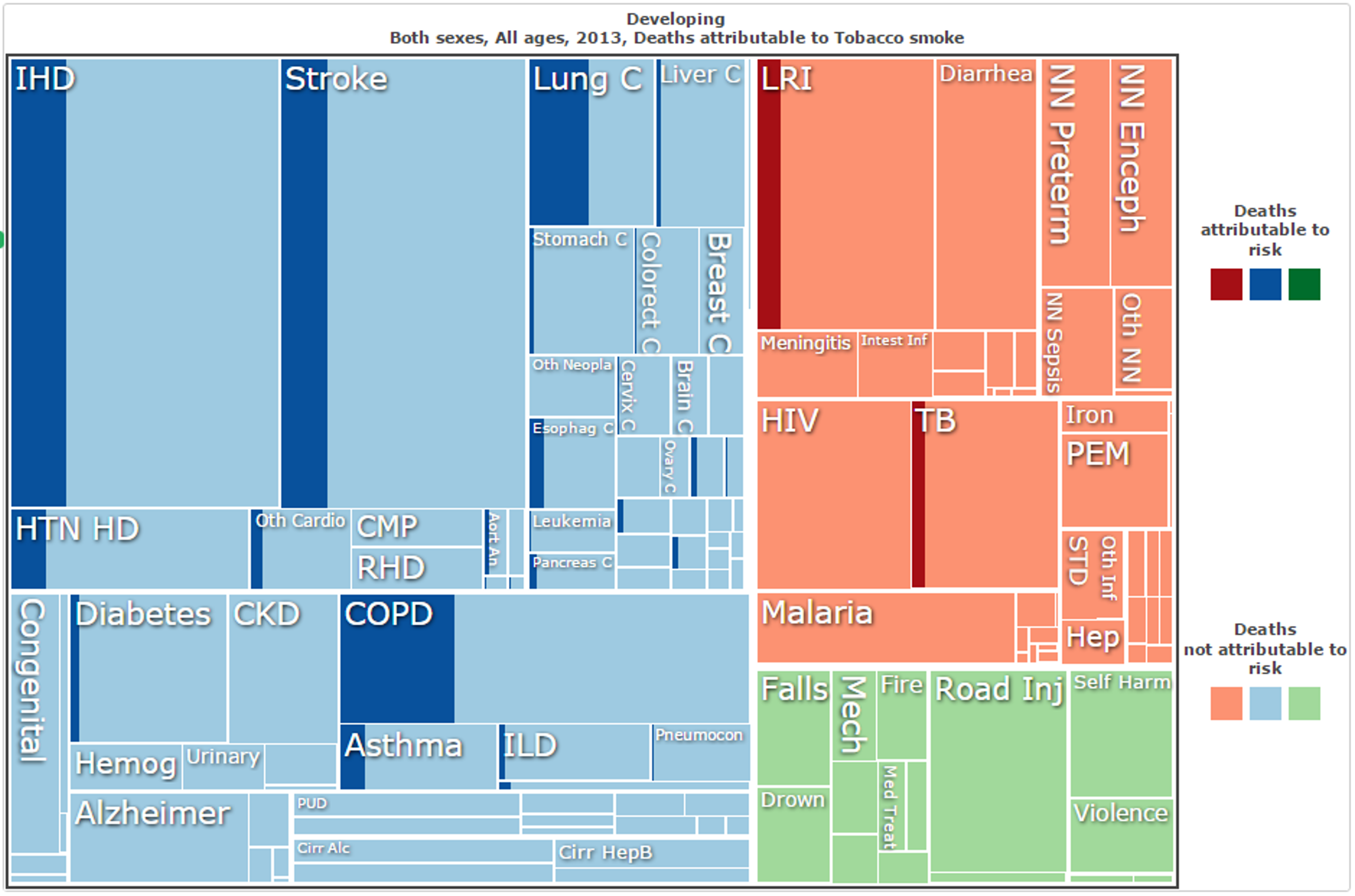
Figure 13: Deaths attributed to tobacco smoke in developing nations in 2013, by cause of death;14
Given the high mortality figures due to tobacco-related conditions, as well as the potential tractability and neglectedness, it is not surprising that tobacco control features on the WHO’s Best Buys list.15 The 2015 Disease Control Priorities 3rd Edition (DCP3), which details highly cost-effective intervention and treatment strategies for various diseases, also recommends tobacco control. It explicitly identifies tobacco taxes, in particular, as “...the most important single cancer intervention at a practical level…”.16
1. How does it work?
The most effective large-scale interventions are primarily those available to national governments - taxation of tobacco, health education, restrictions on sales, advertising and packaging, and various other legislative methods (see Sections 2, 3 and 4 below). For private donors, unable to perform such interventions directly, it is likely that the greatest opportunities lie in funding lobbying and advocacy efforts to encourage government to do so. Funding of awareness campaigns to curb smoking uptake may also be highly effective.
2. Tractability
Tobacco control may be tractable or intractable in two distinct senses: tractable in that certain highly effective policies or initiatives are yet to be implemented (and hence there remain simple improvements which may be made); and tractable in that lobbying efforts and awareness campaigns might be likely to lead to such changes in policy or in general awareness.
Reducing smoking through tax increases, thereby increasing cigarette price, has been shown to be quite tractable on a governmental level, particularly when it comes to reducing smoking amongst young people.17181920 A report by the World Bank estimated that for every 10% increase in cigarette cost, tobacco consumption would drop by 4% in HICs and 8% in LICs (on a global scale, such a 10% increase would hypothetically result in between 240,000 and 480,000 lives saved every year).212223 Young people are also more likely to quit and less likely to start when prices are high.24 The WHO therefore recommends that excise taxes should account for 70% of cigarette cost.25 A report by the Asian Development Bank stated that increasing the price of cigarettes by 50% through taxation would avert 27 million tobacco-related deaths in China, India, Thailand, the Philippines and Vietnam alone.26
Alongside price increases, education and awareness campaigns are methods of reducing tobacco use which appears quite tractable. The WHO Global Adult Tobacco Survey for China showed that only 23% of Chinese adults knew that smoking caused lung cancer, heart attacks and strokes.27 Another study, also conducted in China, found that only 40% were aware that smoking causes coronary heart disease, only about 20% were aware that it causes stroke, and only 7% were aware of all eight of the major health effects considered.2829 This lack of awareness affects the poorest in a population in particular, with those who are illiterate unable to read warning labels. Thus, targeted education initiatives (conducted by governments) and awareness campaigns (conducted by either governments or other organisations) may hence be extremely tractable as there is a large portion of the population yet to be reached.
Pictorial warnings are one method of government-initiated awareness-raising which have been used to try and re-balance this inequality in some countries,30 and there is evidence that pictorial warnings significantly improve awareness of dangers of smoking and reduce the number of young people taking up the practice.31 Packaging controls are also important in reducing the impression that some cigarette brands are less harmful than others.32 Unfortunately, however, 125 countries (out of 198) do not require pictorial warnings on tobacco products, and developing nations are significantly overrepresented in this number, suggesting that this is quite a tractable area for improvement in developing nations.
Total advertising bans have also been effective in reducing cigarette consumption,3334 especially in LMICs,35 including bans on smoking in the workplace.3637
Of course, there is the additional issue of the tractability of lobbying and advocacy - while it might be quite tractable to secure health improvements through policy changes, bringing about those changes through advocacy may be less tractable. Tractability and cost-effectiveness are both extremely difficult to estimate for advocacy, due to the comparatively high uncertainty and low chance of success relative to direct health interventions.[^fn-324]38 There has already been some success in tobacco control advocacy in the Philippines39 and elsewhere,4041 though this may not be representative of future efforts. Ideally, given a particular advocacy organisation, we might be able to provide some suggestion of the tractability of their work based on the exact context and the approach they take. Unfortunately, however, we have not identified any promising charitable organisations in this area with a sizeable funding gap and hence are unable to provide such a suggestion (see Section 7).
3. Cost-effectiveness
Research has recently suggested that taxes on tobacco are “...the single most cost-effective way to save lives in developing countries...”.42 DCP3 also explicitly identifies them as “...the most important single cancer intervention at a practical level…” based on their low cost and high effectiveness.43 As mentioned above, The World Bank estimates that for every 10% increase in cigarette cost, tobacco consumption would drop by 4% in HICs and 8% in LICs,44 particularly among young people for whom the lifelong impact is greater. Given this, the WHO recommends that excise taxes should account for 70% of cigarette cost.45
This cost-effectiveness of such an approach has been estimated at $3-$70 per DALY averted,4647 which appears to compare quite favourably to the most effective humanitarian interventions (for example, approximately $95 per DALY averted through insecticide-treated mosquito nets to protect against malaria).48 As for lives saved, one estimate puts the cost of saving a life by diminishing tobacco use at $1462 (5.5 million lives saved over 10 years at an annual cost of $804 million dollars).49 If 1/3 of the lives saved are due to price increases from higher taxes, which probably underestimates the relative impact of this measure, then the cost of saving a life by raising taxes is about $795 (1.8 million lives saved over 10 years at an annual cost of $143 million).50 Again, this appears to rank increased taxation of tobacco among the most effective interventions available, with the Against Malaria Foundation estimated to prevent the death of a child under the age of 5 for every $3,461 donated.51
Mass-media campaigns to raise awareness and dissuade children from smoking have also been assessed as highly cost-effective. Even in the United Kingdom, with relatively low numbers of total smoking deaths (109,000 per year)52 and generally high intervention costs, such campaigns may add a quality-adjusted life year (QALY), on average, for every $71 spent.53 Although measurements of DALYs averted are generally somewhat lower than measurements of QALYs added,[^fn-325] and hence the cost per DALY averted somewhat higher than the cost per additional QALY, this still indicates that the cost per DALY averted through such media campaigns is still impressively low for a developed nation. Given the lack of awareness and greater population of smokers in countries such as India and China (see above), it is extremely likely that the figure for awareness campaigns in developing countries is lower still.
Of course, again, there is the issue of the cost-effectiveness of lobbying and advocacy - while it might be quite cost-effective to secure health improvements through policy changes, bringing about those changes through advocacy may be less effective and more expensive. Like tractability, the cost-effectiveness of advocacy is extremely difficult to estimate, due to the comparatively high uncertainty and sometimes low chance of success.54 Ideally, given a particular advocacy organisation, we might be able to provide some estimate of the cost-effectiveness of their work based on the exact context and the approach they take. Unfortunately, however, we have not identified any promising charitable organisations with a sizeable funding gap working in this area and hence are unable to provide such an estimate (see Section 7).
4. Positive wider impacts
A major factor which may add to the cost-effectiveness specifically of increased tobacco taxation is the use of the revenue raised on public health. Currently, on average, LMIC governments collect $10.74 per capita in revenue from excise taxes on tobacco products but spend only $0.0078 per capita on tobacco control (development assistance provides another $0.011 per capita).55 This may well be justified. Directing just 1% more of these revenues (or $0.1074 per capita) to tobacco control would increase total spending on tobacco control by more than 500%.56 Increasing funding in this way may diminish or even eliminate the need for additional development assistance for tobacco control, including charitable donations, in the long term. In fact, designing policies that directly fund domestic tobacco control or other cost-effective public health interventions could substantially improve the overall cost-effectiveness of tobacco taxes in the short term, while strengthening domestic public health services. Of course, simply increasing excise taxes on tobacco may not necessarily have this effect but, nonetheless, it does have the potential to increase government spending on public health in developing nations, even if only by a small amount.
5. Due diligence: Possible offsetting/negative impacts
Would more funding decrease smoking at the same level of cost-effectiveness?
Tobacco consumption decreases by 4% for every 10% increase in price,57 so if additional funding would achieve higher tax increases over the same time period, it would do even more good. However, it is unclear whether the cost-effectiveness of doing so would remain constant after already achieving several tax increases - does achieving a 20% increase in price costs twice as much as achieving a 10% increase within the same time period, or does it cost half or 4 times or 10 times as much? Advocacy work is particularly vulnerable to this uncertainty - is there a point of diminishing returns, or perhaps some level of taxation beyond which a serious public backlash might occur? This is a difficult question and the answer is unclear.
Are the benefits of tobacco control too far in the future? (If discounted with time, are they still greater than for other interventions?)
It is worth noting, firstly, that whether to discount lives saved (or DALYs averted) with time is a controversial moral question. Secondly, at least one of the estimates given above discounts projected future DALYs at between 3% (the standard rate used by economists) and 10% (a far more conservative estimate), and still claims that tobacco taxation averts DALYs for a maximum of $70/DALY.58 Moreover, even if we accept such a discount rate, increasing tobacco taxes has both short term benefits (for those who quit smoking) and long term benefits (both for those who quit smoking and those who never start.59 Indeed, it has been estimated that minor increases in tax rates could save 5.5 million lives within the first decade (this estimate was for the period from 2006-2015).60
Are tobacco taxes regressive, disproportionately burdening the poor?
This is an important question to ask given that we’re proposing taxes in LMICs on a product used mostly by the poor. However, the evidence strongly suggests that the tax is not regressive. It has been shown that, while poor people smoke more than affluent people, they are also more sensitive to price increases.61 This means they are more likely to smoke less or quit in response to price increases. As a result, most of the health benefits of tobacco taxes will accrue to low-income individuals, while most of the tax burden will be borne by richer smokers who continue to smoke even when the price has increased.6263 Moreover, poorer smokers would quit and actually save money: in China, a tax increase would save people from the lowest income quintile $21 billion (−$83 to $5 billion) and would also provide financial risk protection worth $1·8 billion ($1·2–2·3 billion), mainly concentrated (74%) in the lowest income quintile.64
Do current estimates accurately assess the cost and cost-effectiveness of advocacy for tobacco taxation?
This is the crucial question for effective altruists interested in donating to tobacco tax advocacy. Organizations funding tobacco control pay for political advocacy, institutional support, and research, as well as advocating for tobacco taxes by lobbying and advising politicians and civil servants. Thus it is crucial that we have an accurate estimate of the cost of personnel and material resources necessary to complete a successful campaign. However, it is often difficult to measure the effectiveness of political advocacy,[^fn-1] specifically whether and to what degree the campaign made the difference. And, even when we can measure its effectiveness, we may not be justified in generalizing from one context to another — for example, a successful campaign in Thailand might not be successful or might cost much more in Nigeria. However, rather than generalize, researchers calculate program costs based on general WHO estimates and the strength of a country’s tax and regulation systems and then total the costs for each country.6566 Nonetheless, if we were to evaluate the cost-effectiveness of a particular organization, we would quite reasonably ask for more concrete numbers based on actual past campaigns. This seems particularly important given that tobacco tax advocacy is likely to experience direct opposition from tobacco industry agents.67
6. Neglectedness
Like tractability and cost-effectiveness, neglectedness may vary between government/direct action and lobbying.
In regards to direct action, it appears that tobacco control is indeed relatively neglected, and that there is the capacity for a high marginal impact. Tobacco control is underfunded relative to the harm it causes (see Figure 15 below). HIV/AIDs prevention and treatment received 10 times more funding in LMICs than tobacco control despite the fact that tobacco causes 3 times more deaths in those countries. Of course, without that funding the number of HIV/AIDS deaths would have been higher, but this fact does not negate the relative neglectedness of tobacco control.
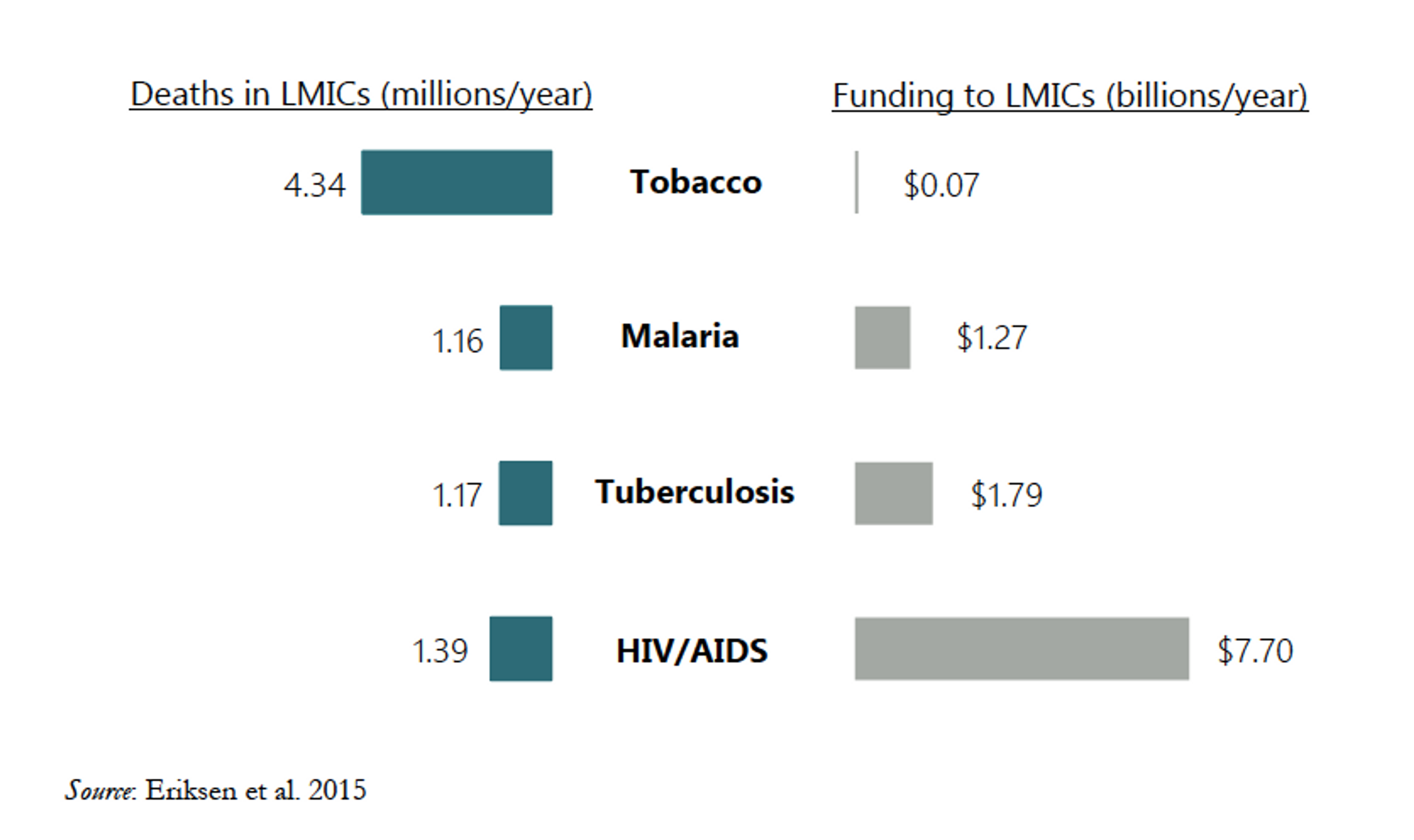
Figure 15: Aid and philanthropic funding relative to deaths for various causes.68
In addition, in regards to lobbying and educational campaigns, tobacco control receives far less funding than the tobacco industry provides for lobbying and promotion of the opposing message. It has been reported that, in the United States alone, more than $20 million was spent on tobacco lobbying in 201569 and approximately $9.6 billion is spent on promotion and advertising.70 This also extends to the developing world, with lobbying, misinformation and lawsuits proving effective in some instances.7172 Given that worldwide lobbying and promotion of tobacco control receive far less than $9.6 billion each year, it might therefore be claimed that this area is still significantly underfunded.
There is still some indication, however, that tobacco control might not be overly neglected. The Bill and Melinda Gates Foundation and Bloomberg Philanthropies have recently begun to fund tobacco control at a higher level (the latter has provided $600 million since 2007).7374 Given the extent of this funding, one might potentially suggest that tobacco control is not a neglected cause. If it remains cost-effective to increase funding, Gates and Bloomberg might be likely to do so. If this is true, then our money would be better spent elsewhere. However, it seems unlikely that these contributions have crowded the area to the point of lowering the marginal impact of donations. Even accounting for Gates’ and Bloomberg’s contributions, tobacco control is certainly not overfunded relative to the harms caused by smoking. Nor is there much evidence to suggest that there is not room for more funding. It has been suggested that Gates and Bloomberg might be “crowding out” other Development Assistance for Tobacco Control (DACT) - after 2006, when Bloomberg and Gates committed to funding tobacco control, some other organizations reduced or ended their funding. However, this drop in funding might be due instead to the effects of the global financial crisis.75
For now, the academic research suggests that spending more would be highly cost-effective. Gates and Bloomberg have contributed $600 million since 2007, which represents about half of total DACT.76 However, one estimate of the amount needed for the four “best buys” in tobacco control, which includes tobacco taxation, is $600 million per year (or $0.11 per capita per year).77 Another estimate puts the cost of decreasing smoking prevalence in key LMICs to 5% by 2040 at $6 billion per year. Tobacco control accounts for about 10% of those costs, or $600 million per year.78 Given that this is the level of funding required annually, there does indeed appear to be a sizeable shortfall in current funding (of approximately $4.2 billion between 2007 and 2015) despite the Gates and Bloomberg contributions.
Given the lack of charities working on such direct action, and that government action is generally not directly funded by private donors, the neglectedness of advocacy and lobbying is perhaps the more relevant factor. This is much more difficult to estimate. A portion of the Gates and Bloomberg contributions is put towards advocacy but it is unlikely to, by itself, be sufficient to cover all promising opportunities. There are also several quite promising charities working on tobacco control advocacy, which appear to be relatively well-funded - the Campaign for Tobacco-Free Kids,79 the World Lung Foundation,80 the International Union Against Tuberculosis and Lung Disease,81 and the Resource Centre for Tobacco Free India.82 The Campaign for Tobacco-Free Kids runs on an annual budget of $18.23 million,83 while the World Lung Foundation has a program budget of $32.3 million,8485 the International Union Against Tuberculosis and Lung Disease has received more than $500 million in funding since 2000,86 and the Resource Centre for Tobacco Free India does not appear to directly solicit donations (nor does its parent organisation, the Voluntary Health Association of India).87 It therefore does not appear that that these organisations are especially neglected, as this indicates that their combined annual funding already exceeds the $70 million in total global aid and philanthropic funding to directly deal with the health effects of tobacco in LMICs.88
7. Charities working in this area
Of the charities we identified in this area as fairly promising, none appeared to have a sizeable funding gap and also agreed to provide information for this report. As mentioned above, among the most promising charities considered were:
- the Campaign for Tobacco-Free Kids;
- the World Lung Foundation;
- the International Union Against Tuberculosis and Lung Disease;
- the Resource Centre for Tobacco Free India / Voluntary Health Association of India;
- as well as Action on Smoking and Health, a formerly taxpayer-funded charity which works on anti-smoking advocacy and lobbying specifically within the United Kingdom.
Unfortunately, we do not have sufficient information to identify any of these organisations as both highly cost-effective and underfunded - despite contacting those which appeared promising, we were unable to obtain sufficient detail from them to demonstrate a level of marginal cost-effectiveness to rival our top recommended charities (see Section 5.1). Although tobacco control is an extremely promising intervention area, with cost-effectiveness estimates to rival our top recommended charities and severe negelectedness in overall funding (specifically, a $4.2 billion shortfall), we cannot currently recommend any particular charities through which there is a good opportunity for donations to have a large impact.[^fn-1]: "The Elusive Craft of Evaluating Advocacy | Stanford Social ..." 2015. 1 Apr. 2016 http://ssir.org/articles/entry/the_elusive_craft_of_evaluating_advocacy