Giving What We Can gives its support to the Against Malaria Foundation, and the intervention of combating malaria more broadly, as one of the most effective ways to fight poverty today. Malaria is estimated to cost Africa $12 billion a year through healthcare and loss of work and education. It accounts for almost one million deaths a year, being a significant contributor to child mortality.
As malaria is intimately related with poverty, eradication of malaria would be a huge step in improving the welfare of lives in developing countries. Smallpox eradication saved more than twice the number of people in the 20th century world peace would have achieved, and saved over $8 billion annually. At a cost of just $1.5 billion, this is one of the most effective aid efforts in history. Eradicating malaria would also have large and far reaching consequences, but innovation and work has been and will be needed.
Despite the current use of insecticide treated bednets and malaria drugs, it is likely that reaching malaria eradication will not be possible without the existence of a vaccine. Vaccines against malaria have been in development for many decades, and receive a huge amount of funding and media coverage. However, to date there is no vaccine available for parasitic infections, such as malaria, and the task is proving to be a huge challenge with many already failed attempts.
Malaria vaccines
Malaria vaccines have received a significant amount of press coverage in the last few months as one vaccine in development by GlaxoSmithKline is showing promising results. The BBC reported the results of a large 18 month phase 3 trial last week: The trial was to detect the effect of the vaccine on 15,000 infants and children in 7 African countries. The trial revealed that malaria cases were reduced by 46% in children, and reduced by 27% in infants. The vaccine has been in development for three decades, and a request for global approval has now been submitted by GSK to the European Medicine’s Authority.
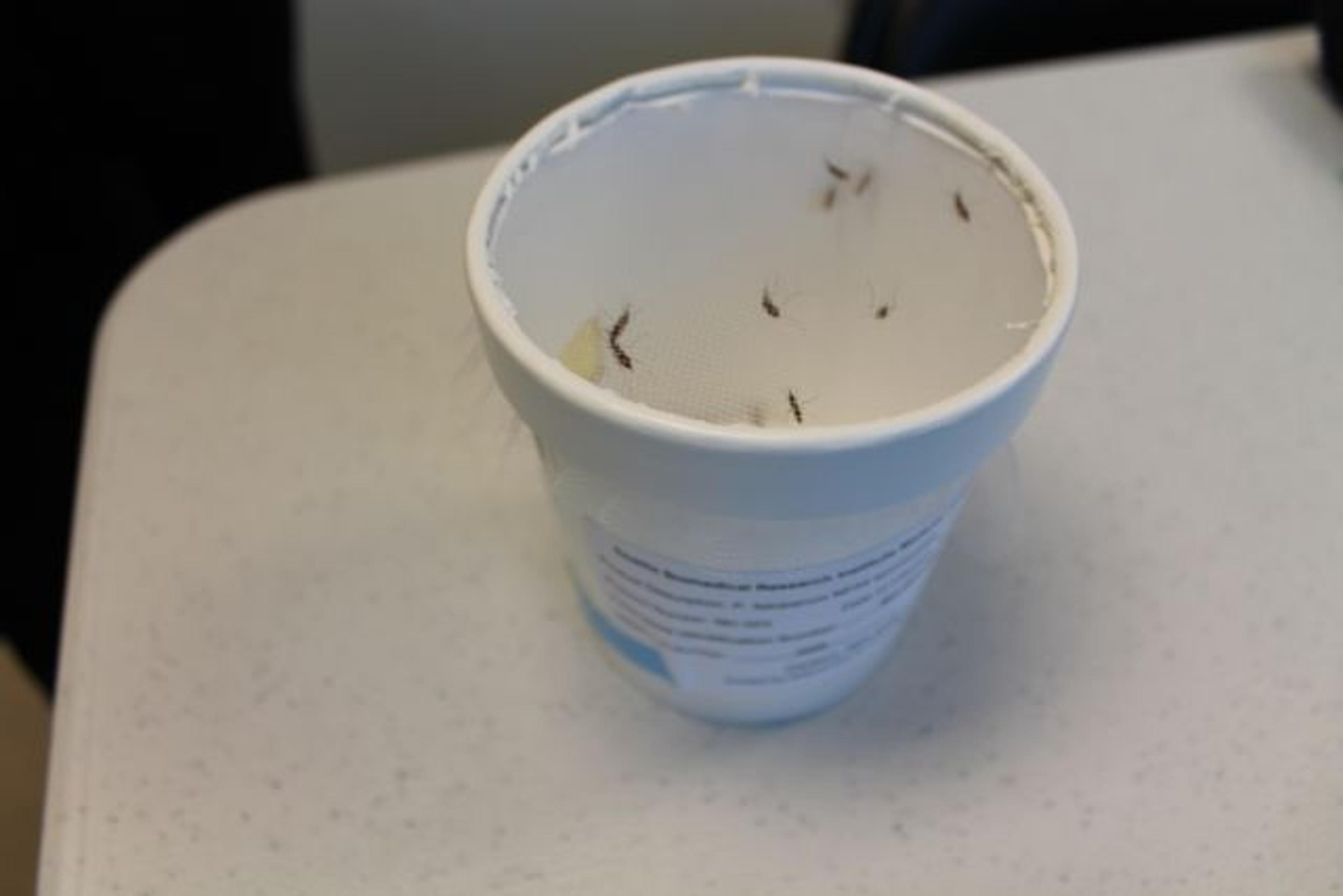
The vaccine used is RTS,S (or Mosquirix as it is known commercially), engineered using genes from the outer protein of Plasmodium falciparum, the malaria parasite, and a portion of the hepatitis B virus, as well as a chemical adjuvant to boost the immune system response. It is the most recently developed recombinant vaccine against malaria, and has proved the most effective to date.
The big players in the efforts to bring a malaria vaccine into use include GlaxoSmithKline, who are already active with the Global Alliance to Eliminate Lymphatic Filariasis, and endorse the London Declaration on Neglected Tropical Diseases, donating 400 million albendazole tablets each year to fight NTDs. The PATH Malaria Vaccine Initiative supports several malaria vaccine candidates, as well as including a drug development programme, currently advancing a synthetic form of the malaria drug artemisinin. The Bill and Melinda Gates Foundation is also a key funder in the development of the vaccine.
What this means for donors
The progress towards a vaccine against malaria is very exciting and we anticipate that when an effective vaccine appears, it has the potential to be a very high impact intervention in poverty reduction. Due to the profile such a vaccine would receive, it is likely that it will also be very well funded. Were an eradication effort to be made against malaria, it is anticipated that a strategic combination of bednets, drugs and vaccines will be what is needed to eradicate the disease. As a result, malaria bednet distribution charities look to be one of the most promising areas for individual donors in the next few years. We look forward to seeing more progress in this area, and anticipate the day when malaria eradication is a feasible possibility.