Estimates of the cost-effectiveness of malarial prevention have tended to focus on the number of deaths which can be averted. Givewell currently estimates that it costs $2,838 to avert one death from malaria.
There may however be supplementary reasons to favour these interventions. In particular, improving the health of the population has important knock-on effects on economic productivity. This post gives an overview of the evidence regarding the extent to which fighting malaria can lead to economic growth and the various mechanisms by which this may occur.
Assessing the aggregate economic system-wide effects of health interventions is a difficult process and as a result there remains considerable uncertainty about the overall economic impact of malaria reduction. Nevertheless, we believe that, on balance, it seems likely that reducing malaria prevalence may have a substantial positive impact on long term productivity through a mechanism analogous to that of mass deworming.
Developmental, educational and cognitive effects: Getting malaria as a child substantially affects lifetime income
Recently, there has been increased attention on the long term productivity impact of having malaria early in life. This is similar to the case for deworming and potentially hugely important. There are a number of plausible mechanisms by which getting malaria early in life could have a long term impact on future earnings:
- Malaria exposure impacts cognitive performance directly12
- Malaria in pregnant women produces anemia which is associated with worse cognitive development34
- Disruption to education caused by malaria may have a long term impact on future earnings5
- Catastrophic health expenditures may limit resources which can be invested in human capital by the family
The long timescales involved and the many confounding factors makes the extent of this impact difficult to evaluate.
One important study by Bleakley (2010) uses a difference-in-differences method to compare the average yearly income of cohorts born shortly before and after malaria eradication campaigns in Latin America and the USA. It found that cohorts born after the anti-malaria campaign in infected areas earned approximately 25% more than the previous generation, after controlling for the differences between cohorts in malaria-free areas. The equivalent number for the USA was 12%.6
These are very substantial results (the increases apply to the whole population rather than just those infected with malaria) but have limited external validity because the data examined were from Latin America and the US (where the predominant strain of malaria differs substantially in its effects to the predominant strain of malaria in Sub-Saharan Africa7), and the 1920s in the US and 1950s in Latin America (when the economic ecosystem was very different).
An additional study by Barofsky (2011) in Uganda found that malaria eradication produced 0.3 more years of schooling in the intervention area compared to the rest of Uganda, which corresponds to an annual income gain of between 3% and 11% depending on the conversion rate used5. While these effects are less substantial than the Bleakley paper they are important for two reasons. First, they have greater external validity in Sub Saharan Africa. Second, because the prevalent strain of malaria in Uganda has a higher mortality rate, the results include the countervailing selection effect of removing lower lifetime income people from the population. Barofsky found that the long term impact of malarial prevention on productivity is substantial, even net of this selection effect. Barofsky’s paper lends credence to the belief that malaria eradication could have long term productivity effects although we would welcome further research in this area.
Costs to individuals and health care system: treating malaria is very expensive, preventing malaria is very cheap
The most direct economic benefit to reduced malaria prevalence is the associated reduction in household health expenditures. Getting malaria is not only deadly but it’s also very expensive. This cost is relatively easy to measure. Household expenditure on malaria treatment in Malawi ranges from about 7% of household income for the average household to 32% of household income for the poorest groups.8 In countries with undeveloped healthcare systems, where out of pocket health expenditures are common, malaria can lead to catastrophic health expenditures and financial impoverishment, even when it is effectively treated.
Where healthcare costs are subsidised, the direct costs of treating malaria fall on the government. The 2015 WHO World Malaria report estimates that, since 2000, 263 million cases of malaria which would have been treated in the public sector have been averted. This is equivalent to a $900m saving for government budgets, of which $610m is attributable to distribution of ITNs/LLINs.9 The 2011 version of the same report noted that “in Rwanda it has been estimated that while it would cost US$ 265 million to sustain the malaria control programme over the next five years, the public health system could avert about US$ 267 million in the costs of diagnosing and treating malaria; and households could avert about US$ 547 million in direct and indirect costs, equivalent to about 7% of household income.”1011
Figure 1: Estimated number of fever cases seen at public health facilities in Africa in 2015 according to different levels of ITN coverage (from WHO malaria report 2011)
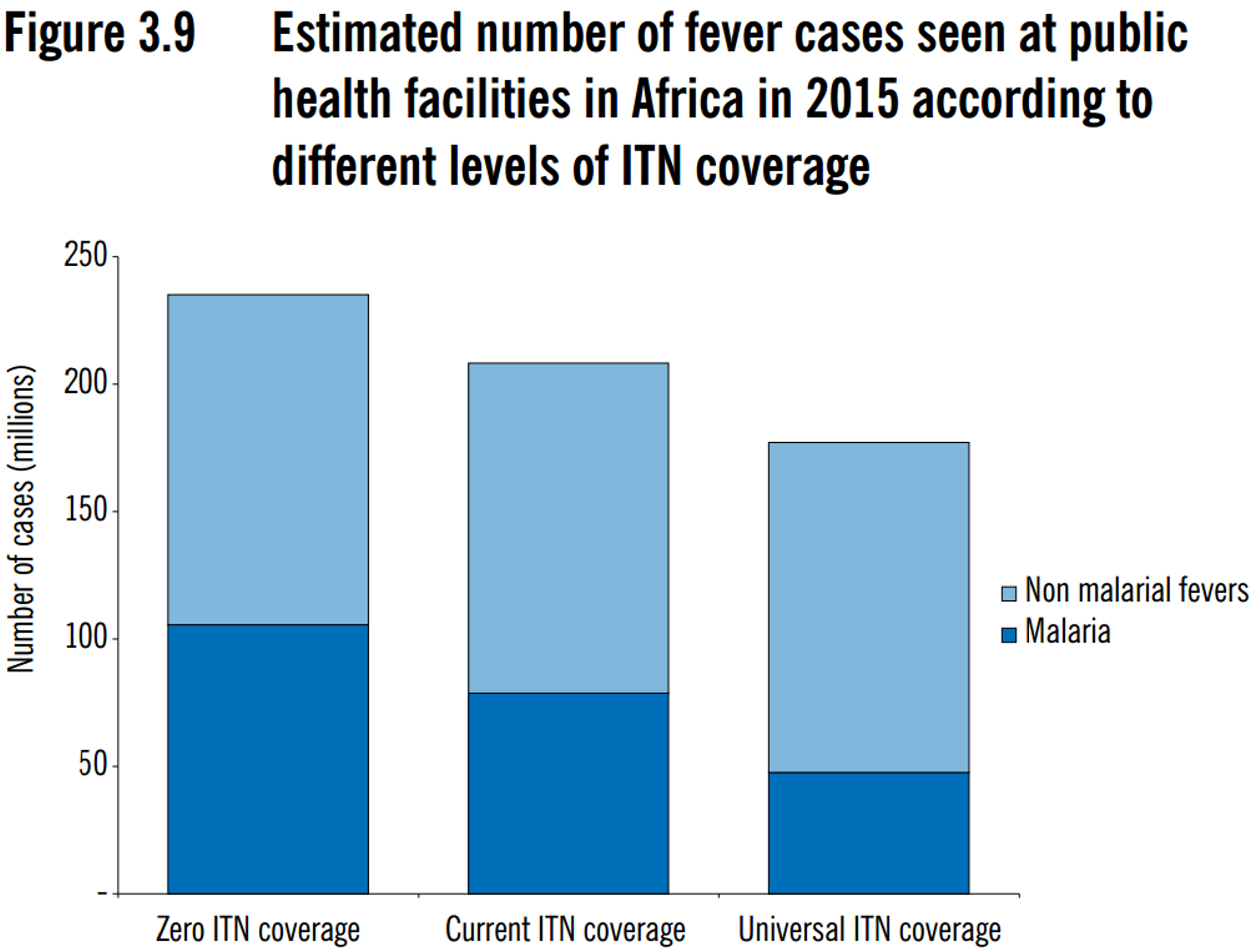
The upshot is that, for a given number of cases prevented/treated, preventative strategies have an advantage over treatment because they avoid catastrophic health expenditures and reduce the burden on the public health system (see Figure 1).
Labour productivity benefits: are people less productive due to malaria?
The economic cost of malaria is not limited to the direct costs of treatment. Working when you are seriously ill is very unpleasant. As a result, the sick take time off work (or at least are less productive) and those with sick children take time off to care for them.
Time lost per episode varies significantly across settings due to the variability of different types of malaria strains, type of economic activity and access to treatment amongst other factors. The average time lost per adult varies between 1 and 5 days.1213 One recent RCT found that a group of farmers who were assigned bednets increased their harvest value by 15%14 (although Givewell have questioned the validity of this result due to baseline imbalances between the treatment and control groups). However, there remains considerable debate as to how much malaria impacts short term productivity. For example, in Malawi, only 52% of adults reported that their illness affected their work.15 Moreover, a larger RCT which looked at 81,597 smallholder contract farmers in 1,507 clusters found no significant impact on cotton production from bednet distribution.16 One possible explanation for this result is that when people are ill they deprioritise less lucrative activities such as basket weaving rather than cotton farming. It seems likely that people who have malaria are less productive in the short term but the scale of this impact is highly uncertain.
Evidence on the macroeconomic effects of malarial eradication
Macroeconomic impact of health improvements is particularly difficult to measure. Early attempts used simple country cross-sectional regressions of health on GDP per capita1718 but these seem doomed to failure because of omitted variable bias and the causal circularity of health and income (improved health may lead to increased income but increased income also leads to improved health). As a result, much of the literature prefers to extrapolate overall macroeconomic impact from microeconomic productivity gains.1920
More promising is the use of time-series data and simulations to evaluate the impact of a health shock on income per capita. Ashraf et al. simulated the impact of the immediate eradication of two diseases, malaria and tuberculosis.21 They found that, while the eradication of tuberculosis may lead to immediate increases in income per capita, the eradication of malaria may lead to short term reductions in income per capita. The difference is explained by the different demographic effects of the two diseases. While tuberculosis primarily affects workers in their prime, malaria disproportionately kills children under the age of 5. Malarial eradication therefore increases the dependency ratio of children to workers in the short term, leading to a fall in income per capita. In the long term, declining endogenous fertility rates, combined with the productivity improvements discussed above mean income per capita rises again (see Figure 2).
Figure 2: Simulated impact of elimination of malaria and tuberculosis on income per capita (from Ashraf et al.)
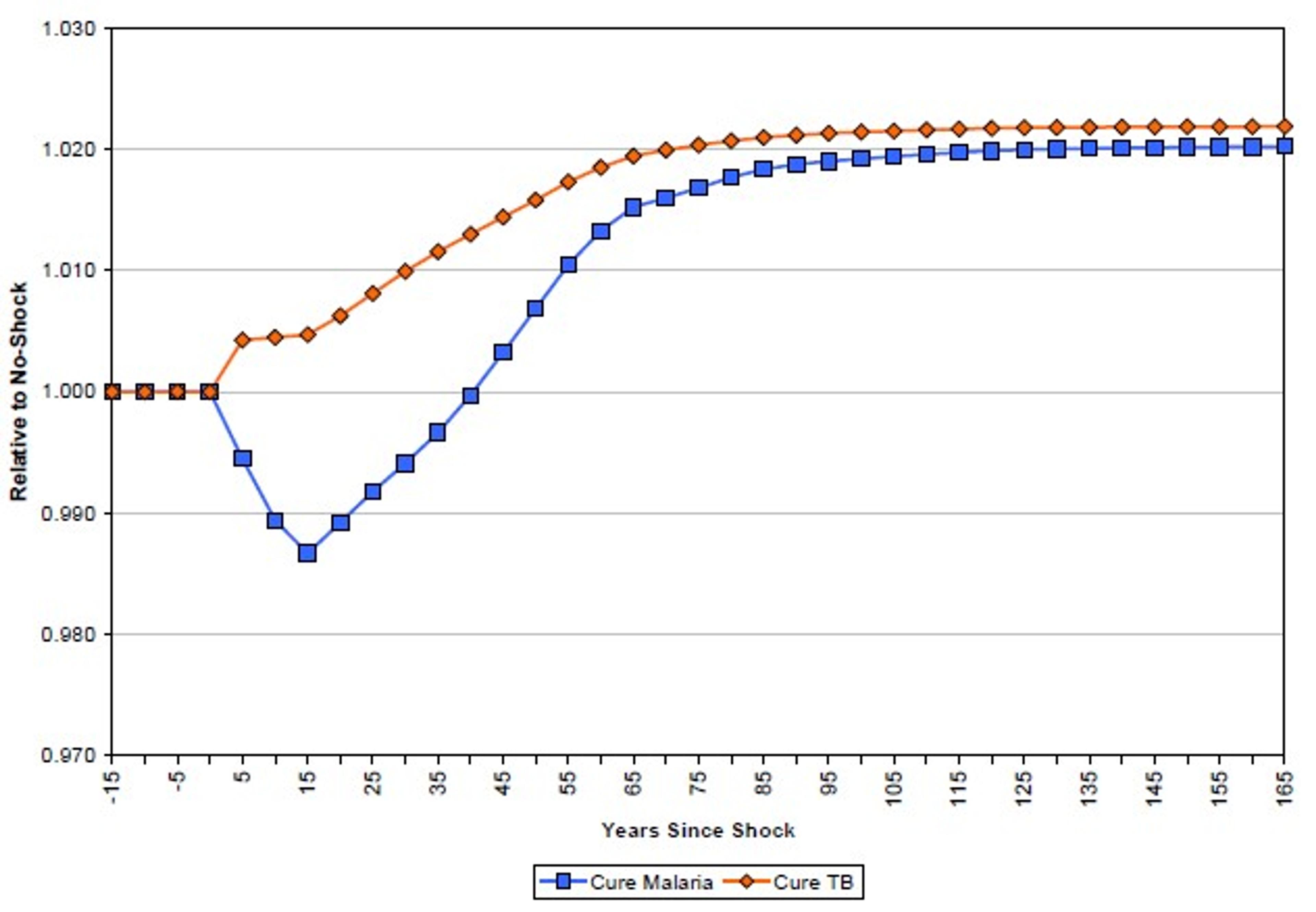
These results have been thoughtfully critiqued by Bleakley.22 While Bleakley agrees that demographic effects mean the impact of malaria eradication is likely to be realised in the long term rather than the short term, he notes, among other things, that the mechanisms through which malaria impacts productivity may not be limited to cases of acute fever (which is assumed by Ashraf et al.) but rather may have more insidious effects on long term productivity. Bleakley concludes that Ashraf’s estimates may be an order of magnitude too low. The debate seems to hinge on the scale of these long term productivity effects, which are discussed above.