Mental Health
Giving What We Can no longer conducts our own research into charities and cause areas. Instead, we’re relying on the work of organisations including J-PAL, GiveWell, and the Open Philanthropy Project, which are in a better position to provide more comprehensive research coverage.
These research reports represent our thinking as of late 2016, and much of the information will be relevant for making decisions about how to donate as effectively as possible. However we are not updating them and the information may therefore be out of date.
Cause Area: Mental Health and Neurological Disorders
Mental health problems impose a very large burden of disease and are relatively neglected, particularly in the developing world. On the other hand, they are generally quite expensive to treat, and so are not as tractable as other cause areas.
We have identified one major charity which focuses on mental health in the developing world, BasicNeeds. BasicNeeds uses a community healthcare model to assist those with mental health problems, their carers, and their families with managing their conditions. While we believe BasicNeeds is a well-run organisation, they do not seem as cost-effective as interventions in other cause areas. We plan to conduct additional research into StrongMinds, another charity which rolls out community based mental healthcare, with a greater focus on depression.
Importance
Figure 1: Overall Global disease burden of all disease as measured by “Disability Adjusted Life Years (DALYs)”. Source: GBD2013
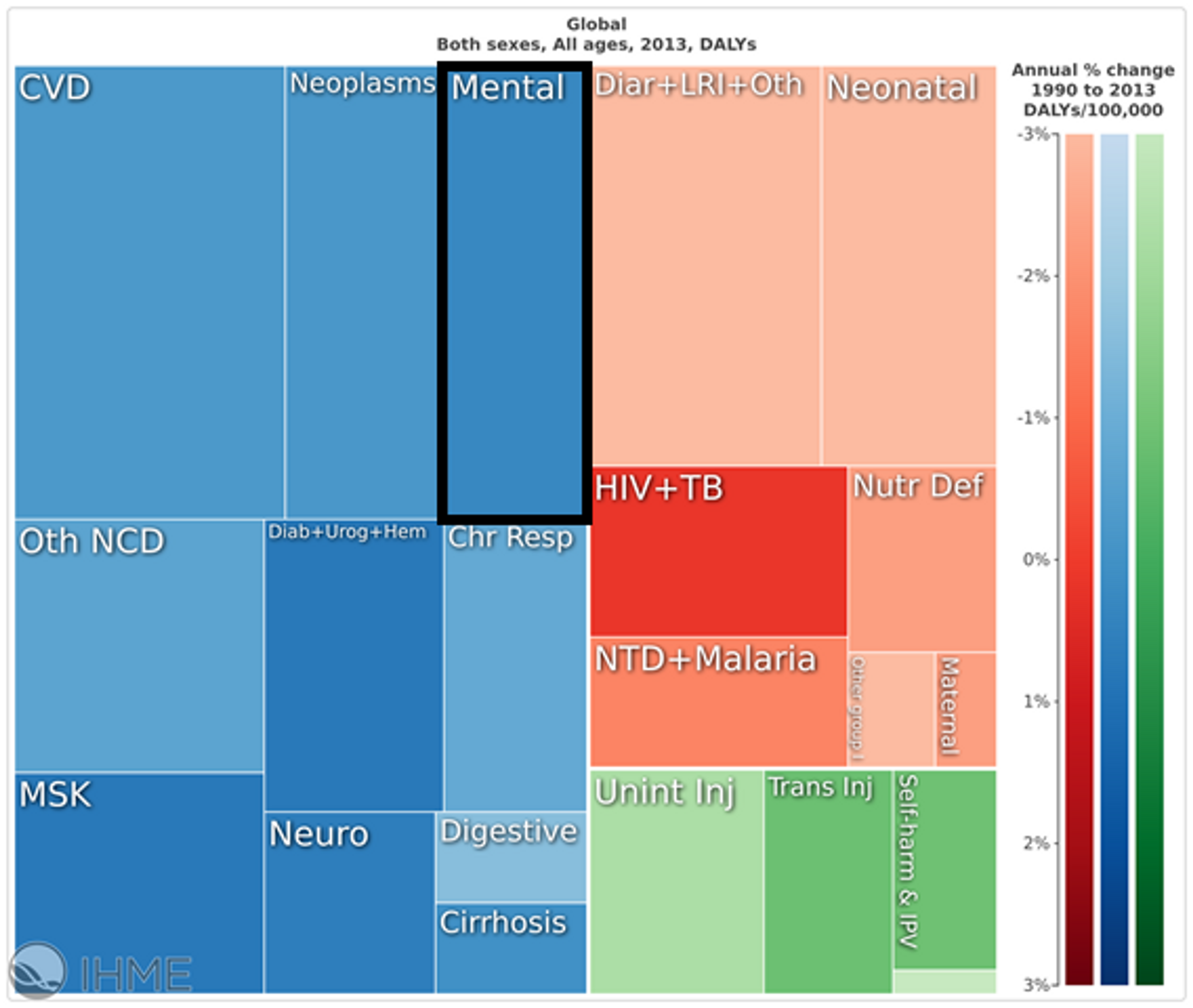
Mental health and substance disorders represent a substantial proportion of the global burden of disease, accounting for approximately 170 million DALYs (7% of the DALY burden worldwide and 6.5% in developing countries) (see Figure 1). Depression, anxiety and drug disorders account for approximately 50% of this burden1.
Neurological diseases (such as Alzheimers, Epilepsy, and Migraine) are categorised separately from mental health and make up an additional 3.5% of the DALY burden. DALYs are a combined measure of morbidity and mortality but mental health has a greater impact on morbidity, accounting for 21% of years of life lost with a disability (30% if neurological conditions are included) but under 1% (3% with neurological conditions) of years of life lost to death.2
Figure 2: Mental health disorders and substance abuse are an increasing proportion of the burden of disease in developing countries. Source: GBD2013
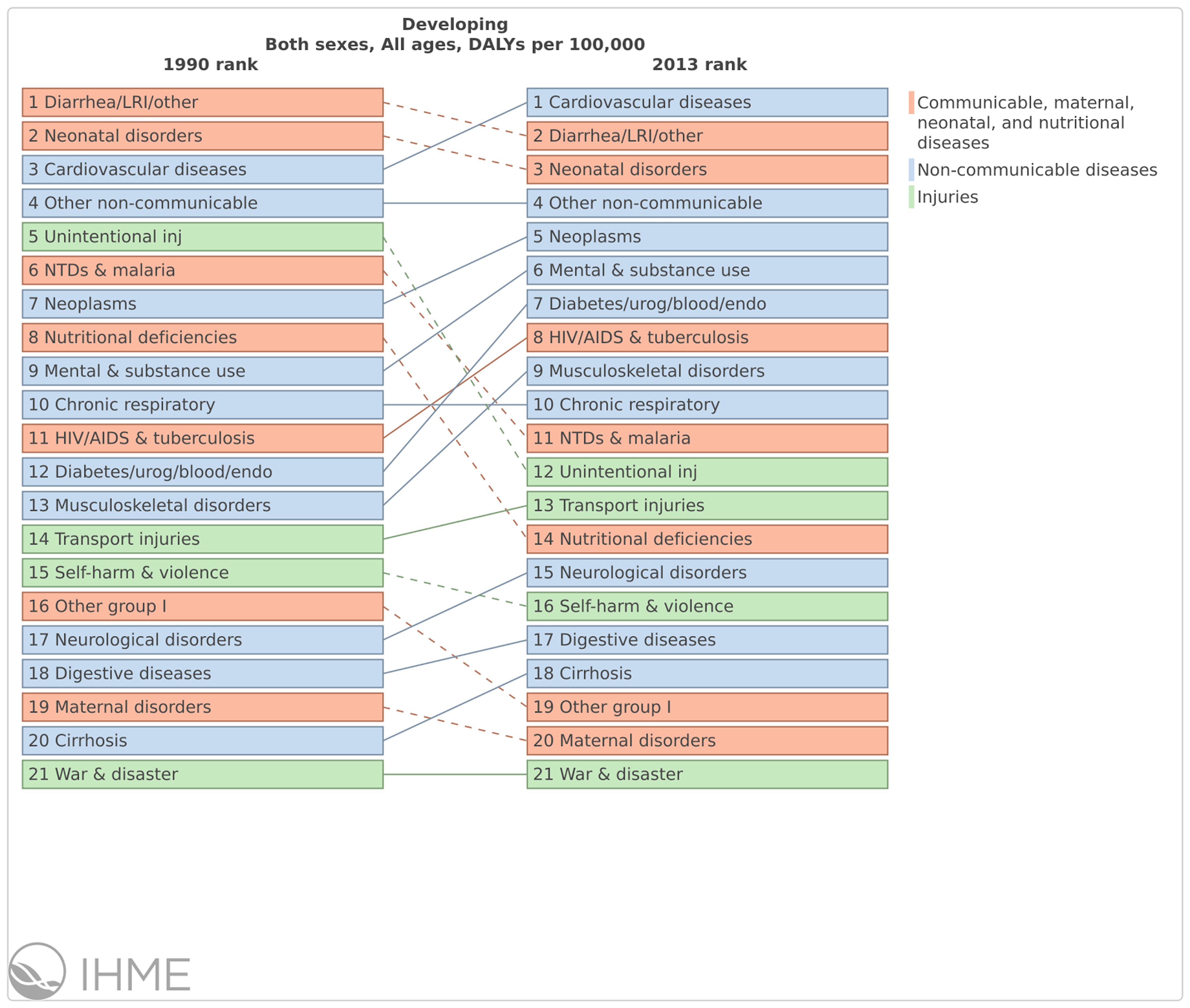
Mental and substance abuse disorders are on the rise and in 2013 contributed the sixth largest burden of disease (see Figure 2). Part of this epidemiological transition is due to success in preventing and treating diseases that cause mortality.
Mental disorders are also associated with some of most serious human rights abuses committed in lower and middle income countries (LMIC), both within families and communities (sexual abuse, forced restraint) and by governments (forced sterilization or incarceration).3
Neglectedness
Mental health is neglected in both developed and developing countries but relatively more neglected in developing countries. Despite a substantial literature on effective interventions, mental health is starkly neglected by the governments of low and middle income countries (LMIC). According to de Menil, a consultant at the Center for Global Development, “one third of LMIC do not have a designated budget for mental health… and among those that do, the average expenditure on mental health in low-income countries is 0.5% of the total health budget.”4 She contrasts the treatment gap in Nigeria – 90% across all diagnosable mental disorders are left untreated– with an average of 32% for schizophrenia to 56-57% for depression and anxiety disorders in European countries.
While philanthropists have supported efforts to address the burden of mental health problems in high-income countries, the international donor community has traditionally neglected mental health disorders. Only 0.7% of development spending is directed at mental health5 - $164 million in 20146 - despite a disease burden of over ten times this scale.
Tractability
Figure 3: Cost-effectiveness estimates for mental health interventions in LMIC. Source: DCP3.
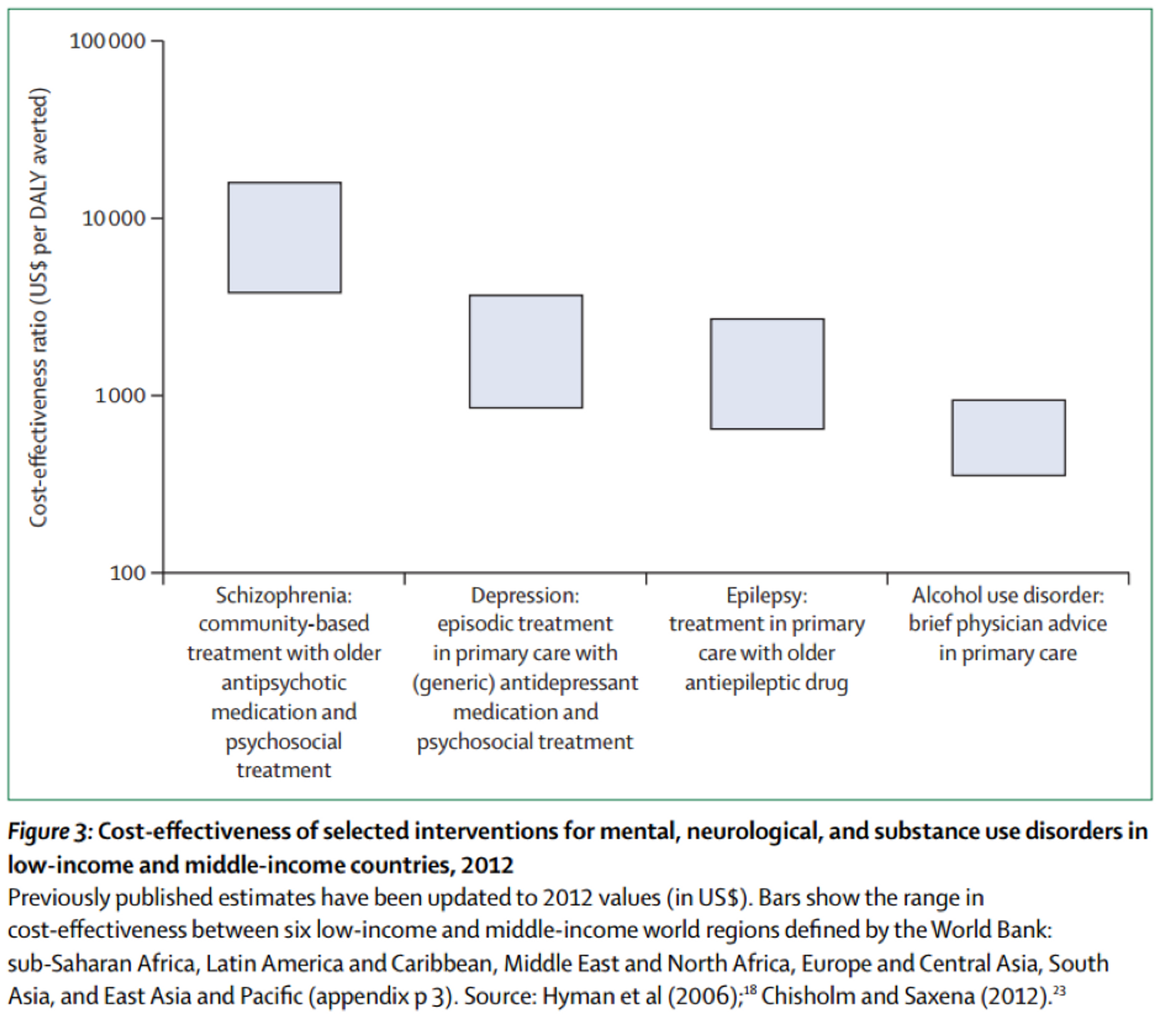
Mental health disorders are treated through a wide range of drug-based, psychological and social interventions. Disease Control Priorities 3, a recent comprehensive review of the cost-effectiveness literature released in October 2015, surveyed studies on cost-effectiveness published between 2007 and 2012. They find that the cost-effectiveness of mental health treatment differs substantially between interventions, with the most cost-effective interventions in terms of $ per DALY averted tending to be brief interventions such as those for alcohol abuse and epilepsy (see Figure 3).7 They note however, that these estimates are highly uncertain as there is a lack of high quality evidence for mental health interventions in LMIC.
The implementation of evidence-based interventions for mental health disorders is generally undertaken at the level of population, community and healthcare platforms rather than as specific vertical interventions. As such, these interventions require careful coordination with the broader health system and so have not tended to be addressed by philanthropic interventions. Middle-income countries such as India and China are scaling up mental health interventions but philanthropic involvement in this area is still limited.8 A recent simulation of the cost-effectiveness of publicly financed epilepsy treatment in India suggested a cost-effectiveness ratio of $190-1790 per DALY averted.9 However, we believe this study has limited external validity for the BasicNeeds (our identified charity) model as it is on a much larger scale ($250m per year for 5 years), includes additional surgical treatment, and relies on a number of health professional which is unrealistic in the regions in which BasicNeeds operates.
The likelihood of developing mental and neurological disorders varies depending on a number of factors. In particular, a recent meta-analysis showed that survivors of cerebral malaria are five times more likely to suffer from epilepsy. We are confident in this meta-analysis as it controlled for publication bias and had a clear criteria for study inclusion.10 As such, we believe that, as preventative measures to reduce malaria are very cost-effective, donating to a charity in this area represents a good opportunity to reduce the burden of mental health disorders in the developing world. Our model suggests that the distribution of long-lasting insecticide treated bednets averts one case of epilepsy for about $25,000. This is comparable to the most cost-effective interventions to treat epilepsy and ignores all other additional benefits (including averting one death from malaria for approximately $3,461).
There are three main ways in which a philanthropist could make a substantial difference in alleviating the burden of mental health disorders:
- Donate to one of the charities currently working on improving mental health in LMIC. The most plausible candidate appears to be BasicNeeds, although limited available data means there is a high degree of uncertainty about the effectiveness of their programs.
- Fund further research into what the most effective interventions in the mental health sphere. A lack of data (e.g. on treatment gaps or the effectiveness of existing interventions) and of highly effective policy recommendations reflect major room for further study of this area, particularly in LMIC. BasicNeeds also does research in this area, providing evidence of the effectiveness of their model to regional and national policymakers to influence mental health policy.
- Treat the causes of mental health problems - address the broader determinants of mental health by donating to a cost-effective programme aimed at economic empowerment or reducing the risk factors of mental or neurological disorders. Malaria is a major risk factor for neurological disorders and there is also evidence that conditional cash transfers contribute significantly to psychological well-being and result in reduced prevalence of depression.