Cancer (Part 2 of 2)
Giving What We Can no longer conducts our own research into charities and cause areas. Instead, we're relying on the work of organisations including J-PAL, GiveWell, and the Open Philanthropy Project, which are in a better position to provide more comprehensive research coverage.
These research reports represent our thinking as of late 2016, and much of the information will be relevant for making decisions about how to donate as effectively as possible. However we are not updating them and the information may therefore be out of date.
Cause Area: Cancer
This report is a continuation of our report on cancer interventions. Part 1 is available here.
5.2 Tobacco control (tracheal, bronchus, and lung cancer)
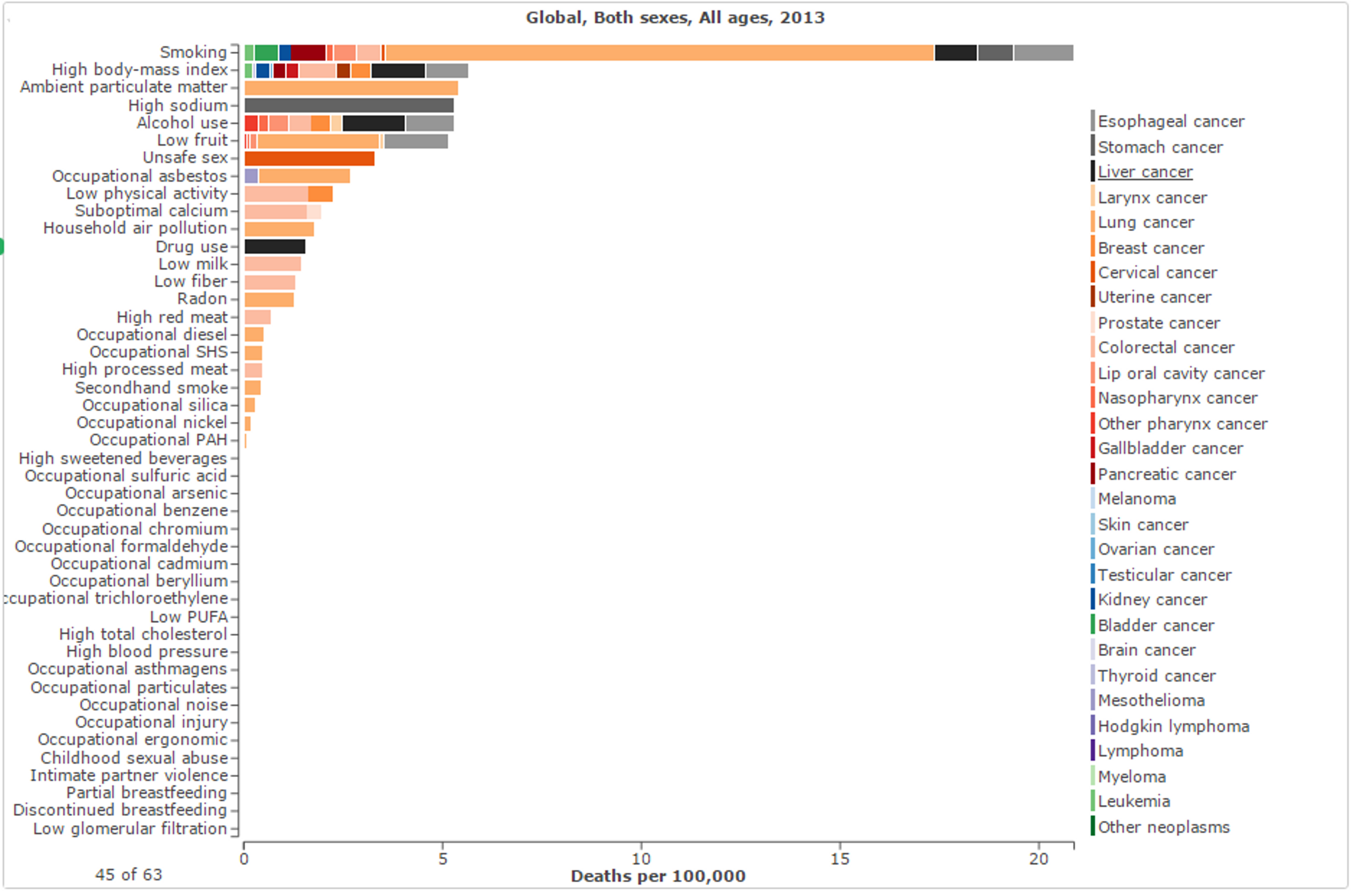
Lung cancer is the single largest contributor to cancer deaths, resulting in 1.59 million deaths each year.1 Tobacco use is the single most important risk factor for cases of lung cancer, to which 70% of those 1.59 million deaths can be attributed.2 In addition, smoking is the single greatest identifiable risk factor for deaths due to all forms of cancer worldwide (see Figure 10), resulting in 20.89 cancer deaths per 100,000 - 2.73% of all deaths worldwide, from any cause.3
Figure 10: Risk factors (all categories) for deaths due to neoplasms in 2013, separated by type of neoplasm;3
Including conditions other than cancer specifically, tobacco kills up to half of all people who use it (i.e. shortens their lifespan), and has a global death toll of almost 6 million people per year (600,000 of whom are non-smokers exposed to secondhand smoke).45 This figure is expected to rise to 10 million deaths per year by the middle of this century.6 In response to these figures and the detrimental effect of tobacco use, a variety of anti-smoking mass media campaigns have been conducted in many developed nations and seem to have resulted in decreases in incidence of lung cancer.7 Meanwhile, however, deaths due to lung cancer are increasing in many developing countries (see Figure 11).891011
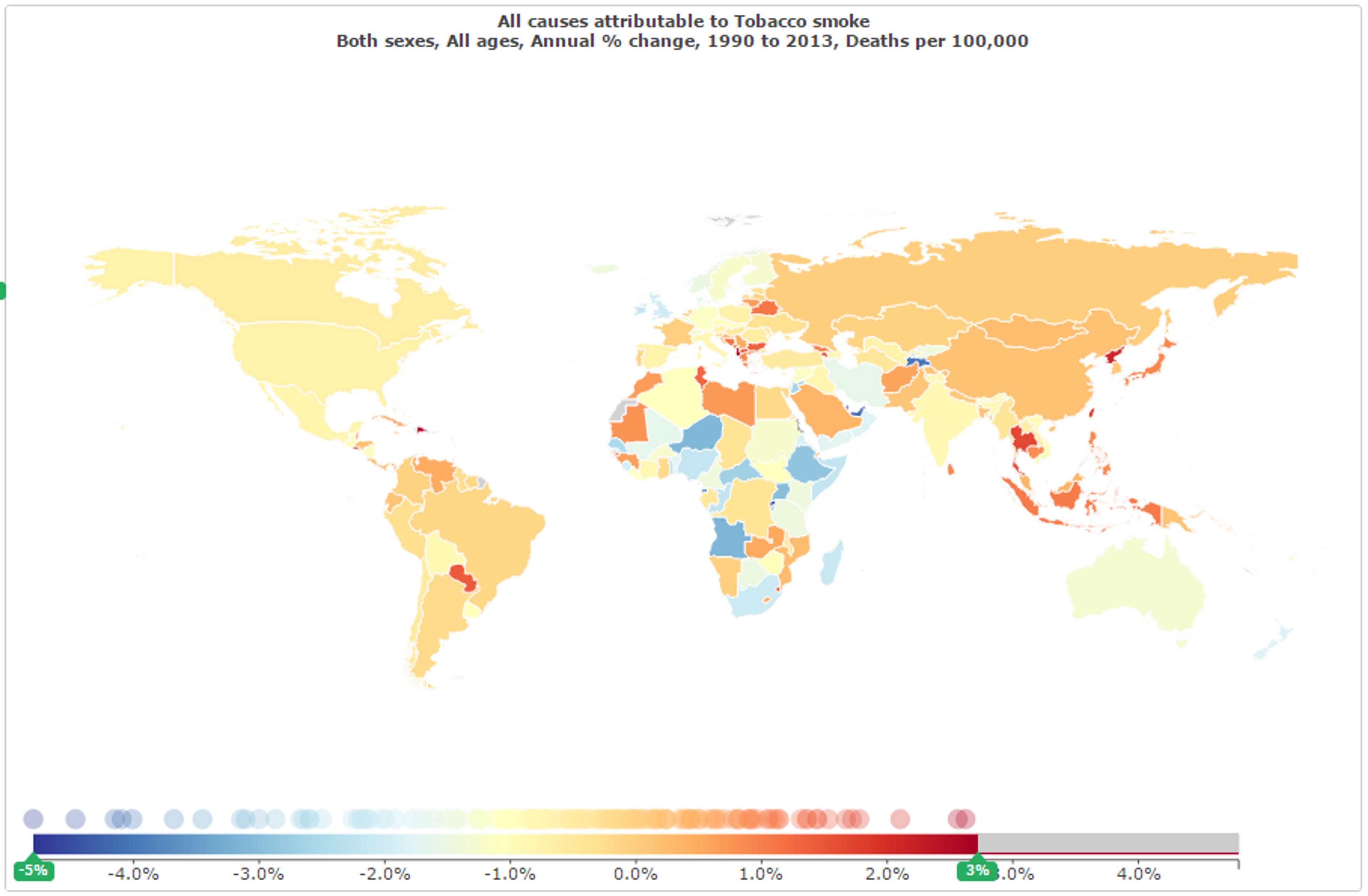
Figure 11: Rate of change of deaths attributed to tobacco smoke between 1990 and 2013;12
The total health burden is also particularly large in developing countries. Due to the uneven distribution of population between developed and developing nations, a large proportion of total deaths due to tobacco use occur in nations such as India and China (see Figure 12). While tobacco and lung cancer may constitute a greater proportion of deaths in developed nations, the absolute number of deaths in nations still in the process of developing provides a problem of greater scale, and hence of potentially much greater impact. Due to the generally lower cost of interventions and neglectedness of public health in these nations, a greater impact can be achieved by improving awareness of and controls on tobacco in these countries than by doing so elsewhere (see Section 5.2.2, 5.2.3, and 5.2.6 below).
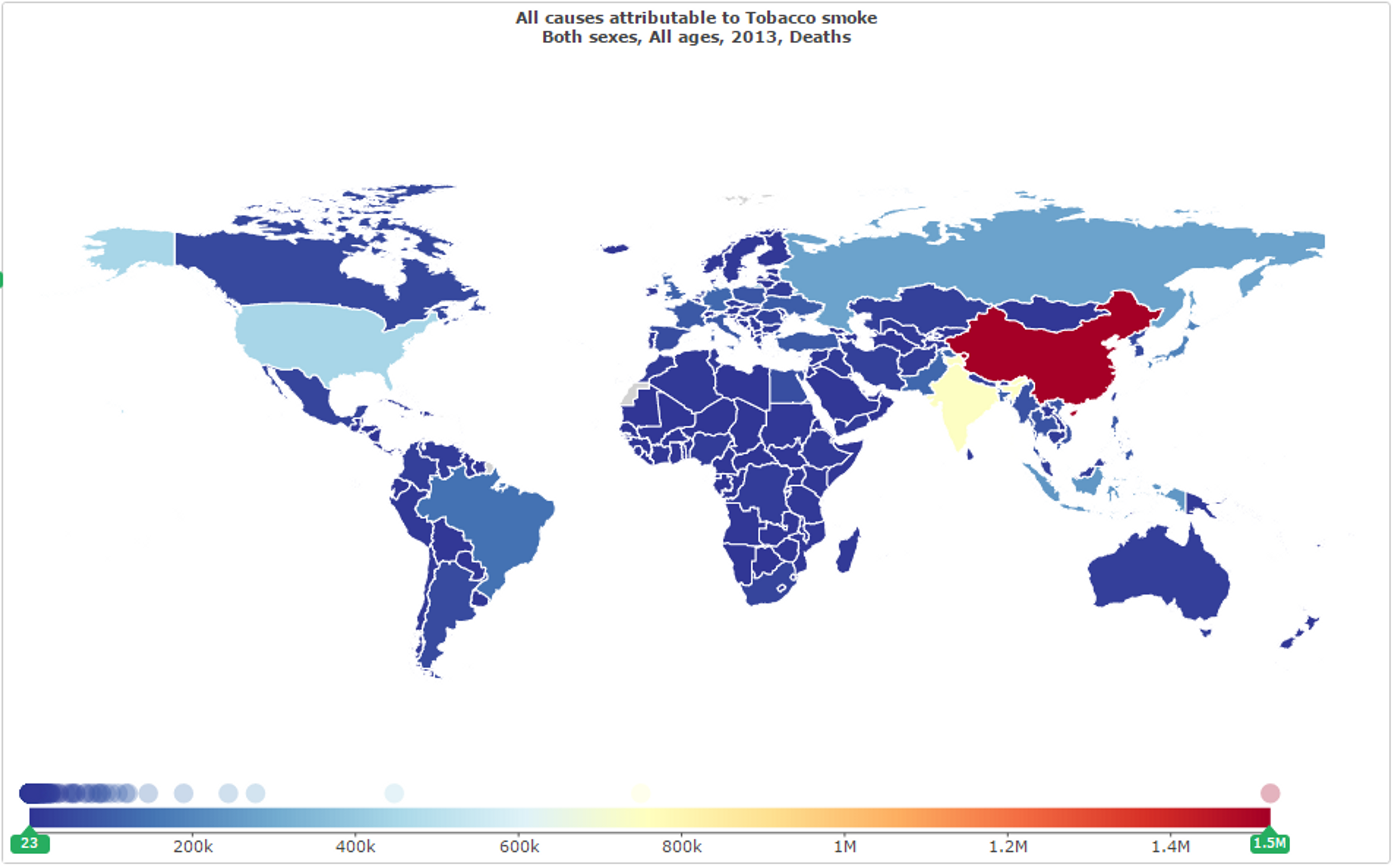
Figure 12: Total deaths attributed to tobacco smoke by country in 2013;13
In developing countries more widely, tobacco use accounts for 9.92% of all deaths (and 4.9% of DALYs incurred), as shown below in Figure 13, which is a greater proportion than all deaths from malaria (2.05%), from HIV (3.1%), from nutritional deficiencies (1.56%), or even from all physical injuries (9.5%).14 These deaths due to tobacco are largely made up of cancer deaths (1.63% of all deaths in developing countries and 16.39% of deaths due to tobacco smoke)15 but also includes various other diseases for which tobacco use increases incidences or chance of death. Similarly for DALYs incurred by tobacco use, 14.73% are due to cancer (0.72% of all DALYs incurred).16 This constitutes several considerable co-benefits of interventions which reduce tobacco use and these co-benefits will be considered in cost-effectiveness estimates below.
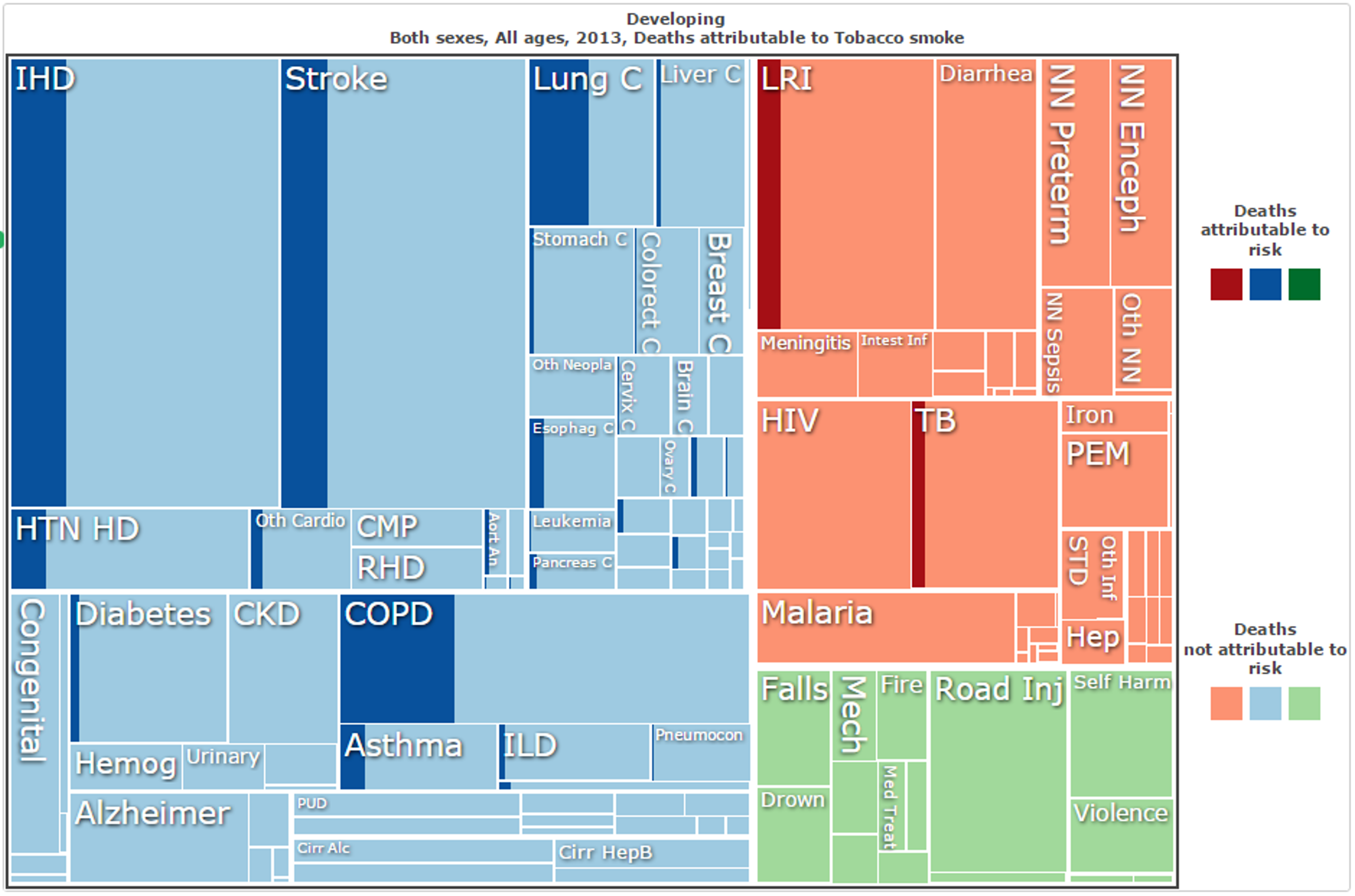
Figure 13: Deaths attributed to tobacco smoke in developing nations in 2013, by cause of death;17
Given the high mortality figures due to lung cancer and also other tobacco-related conditions, as well as the potential tractability and neglectedness, it is not surprising that tobacco control features on the WHO’s Best Buys list.18 The 2015 Disease Control Priorities 3rd Edition (DCP3), which details highly cost-effective intervention and treatment strategies for various diseases, also recommends tobacco control. It explicitly identifies tobacco taxes, in particular, as “...the most important single cancer intervention at a practical level…”.19
5.2.1 How does it work?
The most effective large-scale interventions are primarily those available to national governments - taxation of tobacco, health education, restrictions on sales, advertising and packaging, and various other legislative methods (see Sections 5.2.2, 5.2.3 and 5.2.4 below). For private donors, unable to perform such interventions directly, it is likely that the greatest opportunities lie in funding lobbying and advocacy efforts to encourage government to do so. Funding of awareness campaigns to curb smoking uptake may also be highly effective.
5.2.2 Tractability
Tobacco control may be tractable or intractable in two distinct senses: tractable in that certain highly effective policies or initiatives are yet to be implemented (and hence there remain simple improvements which may be made); and tractable in that lobbying efforts and awareness campaigns might be likely to lead to such changes in policy or in general awareness.
Reducing smoking through tax increases, thereby increasing cigarette price, has been shown to be quite tractable on a governmental level, particularly when it comes to reducing smoking amongst young people.20212223 A report by the World Bank estimated that for every 10% increase in cigarette cost, tobacco consumption would drop by 4% in HICs and 8% in LICs (on a global scale, such a 10% increase would hypothetically result in between 240,000 and 480,000 lives saved every year, approximately 15% of which would be from cancer).242526 Young people are also more likely to quit and less likely to start when prices are high.27 The WHO therefore recommends that excise taxes should account for 70% of cigarette cost.28 A report by the Asian Development Bank stated that increasing the price of cigarettes by 50% through taxation would avert 27 million tobacco-related deaths in China, India, Thailand, the Philippines and Vietnam alone.29
Alongside price increases, education and awareness campaigns are methods of reducing tobacco use which appears quite tractable. The WHO Global Adult Tobacco Survey for China showed that only 23% of Chinese adults knew that smoking caused lung cancer, heart attacks and strokes.30 Another study, also conducted in China, found that only 40% were aware that smoking causes coronary heart disease, only about 20% were aware that it causes stroke, and only 7% were aware of all eight of the major health effects considered.3132 This lack of awareness affects the poorest in a population in particular, with those who are illiterate unable to read warning labels. Thus, targeted education initiatives (conducted by governments) and awareness campaigns (conducted by either governments or other organisations) may hence be extremely tractable as there is a large portion of the population yet to be reached.
Pictorial warnings are one method of government-initiated awareness-raising which have been used to try and re-balance this inequality in some countries,33 and there is evidence that pictorial warnings significantly improve awareness of dangers of smoking and reduce the number of young people taking up the practice.34 Packaging controls are also important in reducing the impression that some cigarette brands are less harmful than others.35 Unfortunately, however, 125 countries (out of 198) do not require pictorial warnings on tobacco products, and developing nations are significantly overrepresented in this number, suggesting that this is quite a tractable area for improvement in developing nations.
Total advertising bans have also been effective in reducing cigarette consumption,3637 especially in LMICs,38 including bans on smoking in the workplace.3940
Of course, there is the additional issue of the tractability of lobbying and advocacy - while it might be quite tractable to secure health improvements through policy changes, bringing about those changes through advocacy may be less tractable. Tractability and cost-effectiveness are both extremely difficult to estimate for advocacy, due to the comparatively high uncertainty and low chance of success relative to direct health interventions.4142 There has already been some success in tobacco control advocacy in the Philippines43 and elsewhere,4445 though this may not be representative of future efforts. Ideally, given a particular advocacy organisation, we might be able to provide some suggestion of the tractability of their work based on the exact context and the approach they take. Unfortunately, however, we have not identified any promising charitable organisations in this area with a sizeable funding gap and hence are unable to provide such a suggestion (see Section 5.2.7).
5.2.3 Cost-effectiveness
Research has recently suggested that taxes on tobacco are “...the single most cost-effective way to save lives in developing countries...”.46 DCP3 also explicitly identifies them as “...the most important single cancer intervention at a practical level…” based on their low cost and high effectiveness.47 As mentioned above, The World Bank estimates that for every 10% increase in cigarette cost, tobacco consumption would drop by 4% in HICs and 8% in LICs,48 particularly among young people for whom the lifelong impact is greater. Given this, the WHO recommends that excise taxes should account for 70% of cigarette cost.49
This cost-effectiveness of such an approach has been estimated at $3-$70 per DALY averted,5051 which appears to compare quite favourably to the most effective humanitarian interventions (for example, approximately $78 per DALY averted through insecticide-treated mosquito nets to protect against malaria).52 As for lives saved, one estimate puts the cost of saving a life by diminishing tobacco use at $1462 (5.5 million lives saved over 10 years at an annual cost of $804 million dollars).53 If 1/3 of the lives saved are due to price increases from higher taxes, which probably underestimates the relative impact of this measure, then the cost of saving a life by raising taxes is about $795 (1.8 million lives saved over 10 years at an annual cost of $143 million).54 Again, this appears to rank increased taxation of tobacco among the most effective interventions available, with the Against Malaria Foundation estimated to prevent the death of a child under the age of 5 for every $3,461 donated.55
It is worth noting that the above estimates include deaths and DALYs incurred by tobacco use through diseases other than cancer. Given that 14.73% of the DALYs attributable to tobacco occur through cancer, and 16.39% of deaths,56 we can roughly estimate the cost-effectiveness of tobacco taxation for cancer prevention specifically. Such an estimate implies that tobacco taxation can avert a DALY, specifically due to cancer, for every $20-$475 spent. Likewise, the above estimated costs of saving a life, from cancer specifically, rise to $8922 and $4851, respectively. These figures still suggest that tobacco control is a highly cost-effective method of both saving lives and averting DALYs due to cancer, even if we ignore the sizeable co-benefits which make up approximately 85% of the total benefit.
Mass-media campaigns to raise awareness and dissuade children from smoking have also been assessed as highly cost-effective. Even in the United Kingdom, with relatively low numbers of total smoking deaths (109,000 per year)57 and generally high intervention costs, such campaigns may add a quality-adjusted life year (QALY), on average, for every $71 spent.58 Although measurements of DALYs averted are generally somewhat lower than measurements of QALYs added,59 and hence the cost per DALY averted somewhat higher than the cost per additional QALY, this still indicates that the cost per DALY averted through such media campaigns is still impressively low for a developed nation. Given the lack of awareness and greater population of smokers in countries such as India and China (see above), it is extremely likely that the figure for awareness campaigns in developing countries is lower still.
Of course, again, there is the issue of the cost-effectiveness of lobbying and advocacy - while it might be quite cost-effective to secure health improvements through policy changes, bringing about those changes through advocacy may be less effective and more expensive. Like tractability, the cost-effectiveness of advocacy is extremely difficult to estimate, due to the comparatively high uncertainty and sometimes low chance of success.60 Ideally, given a particular advocacy organisation, we might be able to provide some estimate of the cost-effectiveness of their work based on the exact context and the approach they take. Unfortunately, however, we have not identified any promising charitable organisations with a sizeable funding gap working in this area and hence are unable to provide such an estimate (see Section 5.2.7).
5.2.4 Positive wider impacts
As mentioned above, and as already incorporated into our cost-effectiveness estimates, cancer makes up only 16.39% of deaths due to tobacco smoke (and 14.73% of DALYs incurred) in developing nations (see Section 5.1). Apart from cancer prevention, tobacco control has sizeable co-benefits including the reduction of ischemic heart disease, stroke, hypertensive heart disease, diabetes, chronic obstructive pulmonary disease, asthma, lower respiratory infections, and tuberculosis (see Figure 14 below).61 Thus, it is perhaps unsurprising that tobacco control is an effective method of not only reducing cancer incidence but also greatly improving health overall. This overall benefit is incorporated into the the cost-effectiveness analysis above (see the previous section).
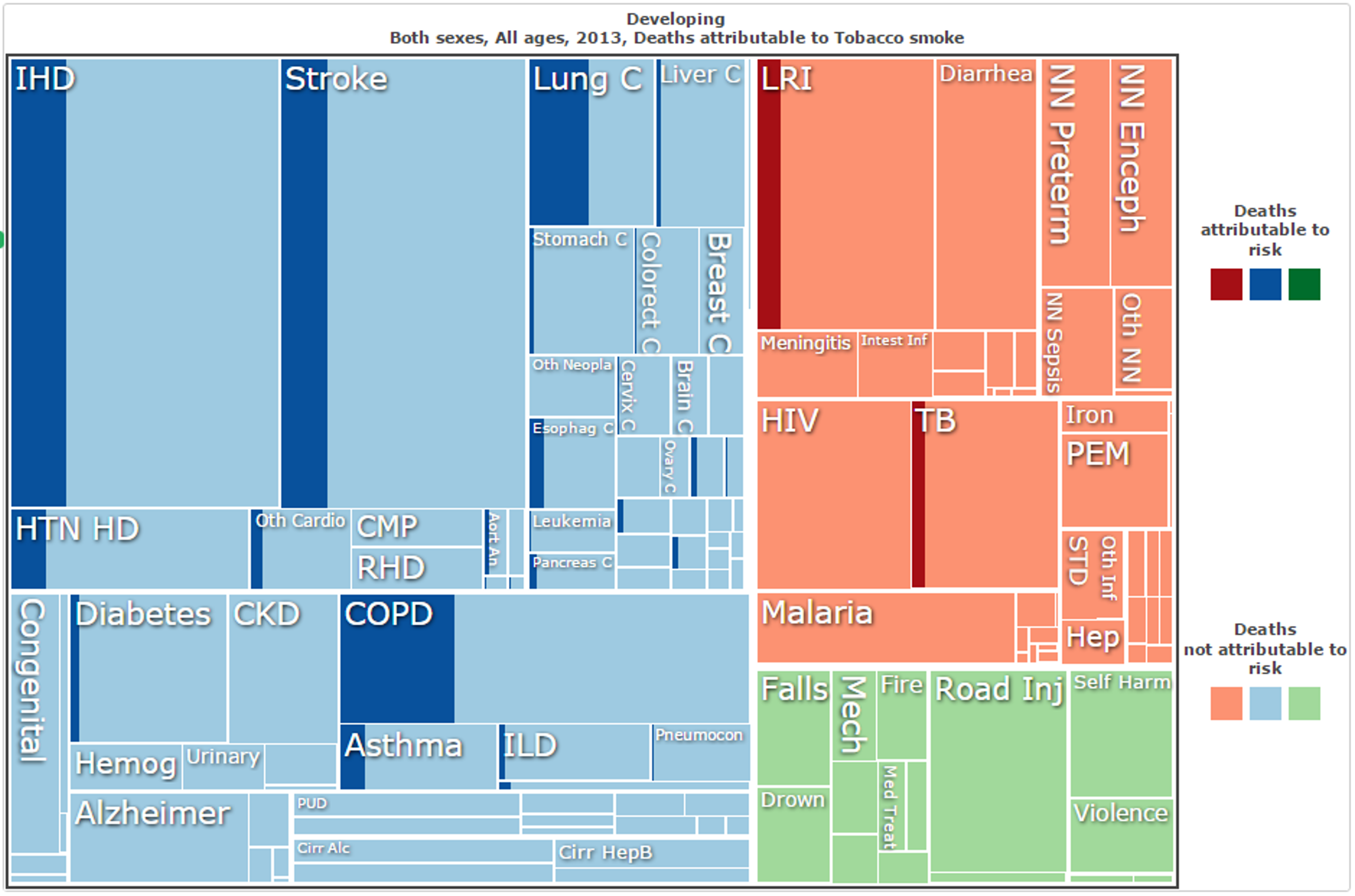
Figure 14: Deaths attributed to tobacco smoke in developing nations in 2013, by cause of death;62
In addition, although not included in the analysis in the previous section or in Figure 14, smoking is a major risk factor for Alzheimer’s disease and dementia more broadly (see our report on dementia for more information).
Another major factor which may add to the cost-effectiveness specifically of increased tobacco taxation is the use of the revenue raised on public health. Currently, on average, LMIC governments collect $10.74 per capita in revenue from excise taxes on tobacco products but spend only $0.0078 per capita on tobacco control (development assistance provides another $0.011 per capita).63 This may well be justified. Directing just 1% more of these revenues (or $0.1074 per capita) to tobacco control would increase total spending on tobacco control by more than 500%.64 Increasing funding in this way may diminish or even eliminate the need for additional development assistance for tobacco control, including charitable donations, in the long term. In fact, designing policies that directly fund domestic tobacco control or other cost-effective public health interventions could substantially improve the overall cost-effectiveness of tobacco taxes in the short term, while strengthening domestic public health services. Of course, simply increasing excise taxes on tobacco may not necessarily have this effect but, nonetheless, it does have the potential to increase government spending on public health in developing nations, even if only by a small amount.
5.2.5 Due diligence: Possible offsetting/negative impacts
Would more funding decrease smoking at the same level of cost-effectiveness?
Tobacco consumption decreases by 4% for every 10% increase in price,65 so if additional funding would achieve higher tax increases over the same time period, it would do even more good. However, it is unclear whether the cost-effectiveness of doing so would remain constant after already achieving several tax increases - does achieving a 20% increase in price costs twice as much as achieving a 10% increase within the same time period, or does it cost half or 4 times or 10 times as much? Advocacy work is particularly vulnerable to this uncertainty - is there a point of diminishing returns, or perhaps some level of taxation beyond which a serious public backlash might occur? This is a difficult question and the answer is unclear.
Are the benefits of tobacco control too far in the future? (If discounted with time, are they still greater than for other interventions?)
It is worth noting, firstly, that whether to discount lives saved (or DALYs averted) with time is a controversial moral question. Secondly, at least one of the estimates given above discounts projected future DALYs at between 3% (the standard rate used by economists) and 10% (a far more conservative estimate), and still claims that tobacco taxation averts DALYs for a maximum of $70/DALY.66 Moreover, even if we accept such a discount rate, increasing tobacco taxes has both short term benefits (for those who quit smoking) and long term benefits (both for those who quit smoking and those who never start.67 Indeed, it has been estimated that minor increases in tax rates could save 5.5 million lives within the first decade (this estimate was for the period from 2006-2015).68
Are tobacco taxes regressive, disproportionately burdening the poor?
This is an important question to ask given that we’re proposing taxes in LMICs on a product used mostly by the poor. However, the evidence strongly suggests that the tax is not regressive. It has been shown that, while poor people smoke more than affluent people, they are also more sensitive to price increases.69 This means they are more likely to smoke less or quit in response to price increases. As a result, most of the health benefits of tobacco taxes will accrue to low-income individuals, while most of the tax burden will be borne by richer smokers who continue to smoke even when the price has increased.7071 Moreover, poorer smokers would quit and actually save money: in China, a tax increase would save people from the lowest income quintile $21 billion (−$83 to $5 billion) and would also provide financial risk protection worth $1·8 billion ($1·2–2·3 billion), mainly concentrated (74%) in the lowest income quintile.72
5.2.6 Neglectedness
Like tractability and cost-effectiveness, neglectedness may vary between government/direct action and lobbying.
In regards to direct action, it appears that tobacco control is indeed relatively neglected, and that there is the capacity for a high marginal impact. Tobacco control is underfunded relative to the harm it causes (see Figure 15 below). HIV/AIDs prevention and treatment received 10 times more funding in LMICs than tobacco control despite the fact that tobacco causes 3 times more deaths in those countries. Of course, without that funding the number of HIV/AIDS deaths would have been higher, but this fact does not negate the relative neglectedness of tobacco control.
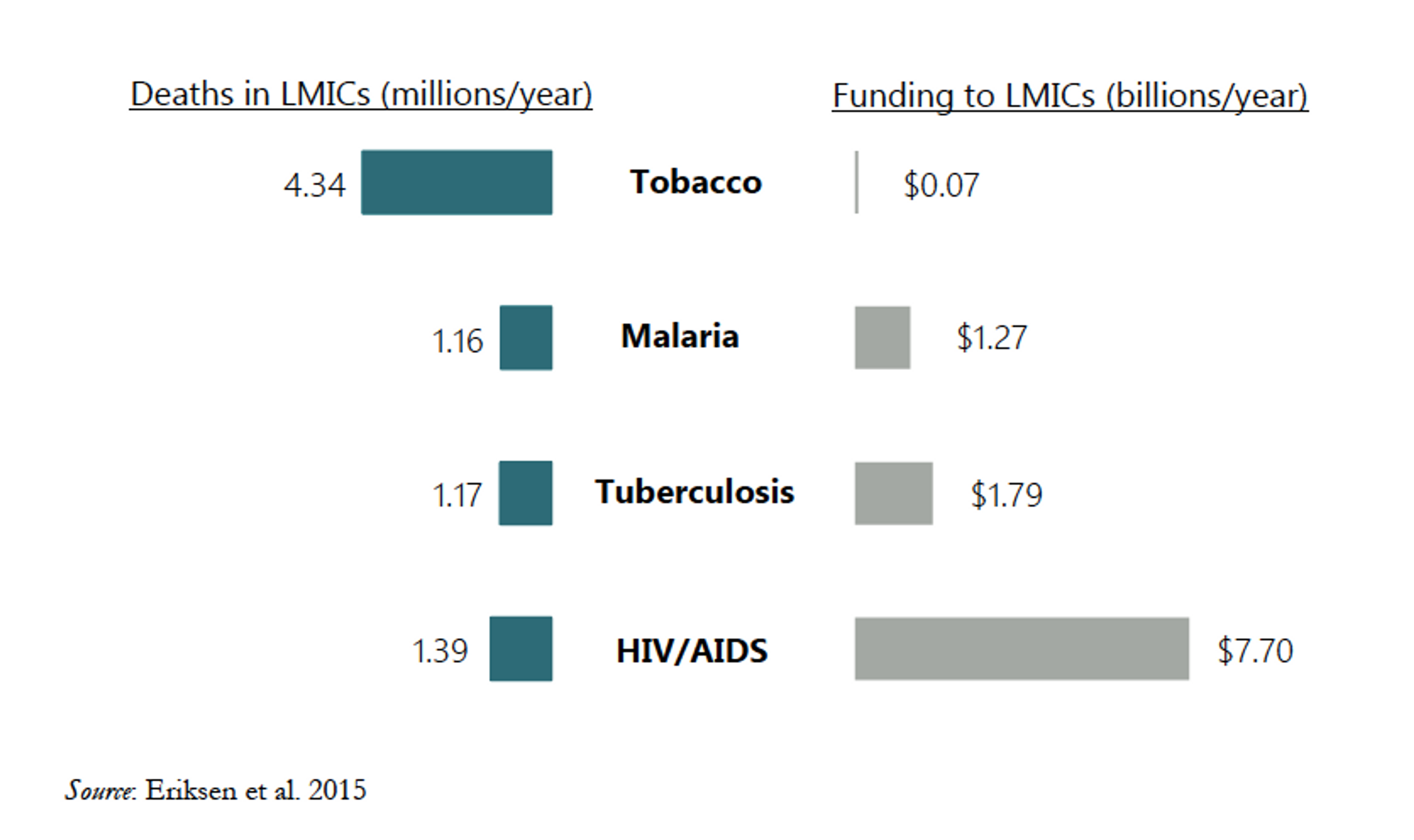
Figure 15: Aid and philanthropic funding relative to deaths for various causes.73
In addition, in regards to lobbying and educational campaigns, tobacco control receives far less funding than the tobacco industry provides for lobbying and promotion of the opposing message. It has been reported that, in the United States alone, more than $20 million was spent on tobacco lobbying in 201574 and approximately $9.6 billion is spent on promotion and advertising.75 This also extends to the developing world, with lobbying, misinformation and lawsuits proving effective in some instances.7677 Given that worldwide lobbying and promotion of tobacco control receive far less than $9.6 billion each year, it might therefore be claimed that this area is still significantly underfunded.
There is still some indication, however, that tobacco control might not be overly neglected. The Bill and Melinda Gates Foundation and Bloomberg Philanthropies have recently begun to fund tobacco control at a higher level (the latter has provided $600 million since 2007).7879 Given the extent of this funding, one might potentially suggest that tobacco control is not a neglected cause. If it remains cost-effective to increase funding, Gates and Bloomberg might be likely to do so. If this is true, then our money would be better spent elsewhere. However, it seems unlikely that these contributions have crowded the area to the point of lowering the marginal impact of donations. Even accounting for Gates’ and Bloomberg’s contributions, tobacco control is certainly not overfunded relative to the harms caused by smoking. Nor is there much evidence to suggest that there is not room for more funding. It has been suggested that Gates and Bloomberg might be “crowding out” other Development Assistance for Tobacco Control (DACT) - after 2006, when Bloomberg and Gates committed to funding tobacco control, some other organizations reduced or ended their funding. However, this drop in funding might be due instead to the effects of the global financial crisis.80
For now, the academic research suggests that spending more would be highly cost-effective. Gates and Bloomberg have contributed $600 million since 2007, which represents about half of total DACT.81 However, one estimate of the amount needed for the four “best buys” in tobacco control, which includes tobacco taxation, is $600 million per year (or $0.11 per capita per year).82 Another estimate puts the cost of decreasing smoking prevalence in key LMICs to 5% by 2040 at $6 billion per year. Tobacco control accounts for about 10% of those costs, or $600 million per year.83 Given that this is the level of funding required annually, there does indeed appear to be a sizeable shortfall in current funding (of approximately $4.2 billion between 2007 and 2015) despite the Gates and Bloomberg contributions.
Given the lack of charities working on such direct action, and that government action is generally not directly funded by private donors, the neglectedness of advocacy and lobbying is perhaps the more relevant factor. This is much more difficult to estimate. A portion of the Gates and Bloomberg contributions is put towards advocacy but it is unlikely to, by itself, be sufficient to cover all promising opportunities. There are also several quite promising charities working on tobacco control advocacy, which appear to be relatively well-funded - the Campaign for Tobacco-Free Kids,84 the World Lung Foundation,85 the International Union Against Tuberculosis and Lung Disease,86 and the Resource Centre for Tobacco Free India.87 The Campaign for Tobacco-Free Kids runs on an annual budget of $18.23 million,88 while the World Lung Foundation has a program budget of $32.3 million,8990 the International Union Against Tuberculosis and Lung Disease has received more than $500 million in funding since 2000,91 and the Resource Centre for Tobacco Free India does not appear to directly solicit donations (nor does its parent organisation, the Voluntary Health Association of India).92 It therefore does not appear that that these organisations are especially neglected, as this indicates that their combined annual funding already exceeds the $70 million in total global aid and philanthropic funding to directly deal with the health effects of tobacco in LMICs.93
5.2.7 Charities working in this area
Of the charities we identified in this area as fairly promising, none appeared to have a sizeable funding gap and also agreed to provide information for this report. As mentioned above, among the most promising charities considered were:
- the Campaign for Tobacco-Free Kids;
- the World Lung Foundation;
- the International Union Against Tuberculosis and Lung Disease;
- the Resource Centre for Tobacco Free India / Voluntary Health Association of India;
- as well as Action on Smoking and Health, a formerly taxpayer-funded charity which works on anti-smoking advocacy and lobbying specifically within the United Kingdom.
Unfortunately, we do not have sufficient information to identify any of these organisations as both highly cost-effective and underfunded - despite contacting those which appeared promising, we were unable to obtain sufficient detail from them to demonstrate a level of cost-effectiveness to rival PHC (see Section 5.1). Although tobacco control is an extremely promising intervention area, with cost-effectiveness estimates to rival our top recommended charities and severe negelectedness in overall funding (specifically, a $4.2 billion shortfall), we cannot currently recommend any particular charities through which there is a good opportunity for donations to have a large impact.
5.3 Hepatitis B vaccination, treatment of parasites (liver cancer, bladder cancer)
Liver cancer has one of the highest mortality rates of any primary cancer. In 2012, it caused 746,000 deaths out of 782,000 cases.94 In addition, 83% of new cases occur in developing countries, where diagnosis and treatment is particularly difficult.95 Some highly cost-effective interventions are available to reduce the number of people who get the disease, as recommended by both WHO and DCP3, and which may have significant co-benefits. Similar interventions are also available for bladder cancer.
To prevent liver cancer, Hepatitis B vaccination is the first line of defence. Hepatitis B is a cancer-causing virus responsible for around 60% of hepatocellular carcinoma (the most common type of liver cancer) in LICs.96 The virus attacks the liver, sometimes setting up an infection which can last for years. 15-45% of those with long-term infection will develop serious complications such as cirrhosis and liver cancer during their lifetime.9798
The majority of countries now aim to vaccinate children at birth, but coverage at birth is still low in some areas.99 Initial vaccination within 24 hours is very important in preventing transmission from mother to child, which often results in dangerous long-term infection.100101 Increasing vaccine coverage would greatly decrease Hep B infection rates and hence liver cancer incidence.102
The WHO has previously found that Hepatitis B vaccinations carried out by the GAVI Alliance avert a disability-adjusted life year (DALY) for approximately US$47.103 This compares favourably with our top recommended charities - for example, the Against Malaria Foundation is estimated to avert a DALY for approximately every $78 in donated funds.104105 However, GAVI is extremely well funded, receiving $4.3 billion in pledged donations for 2011-2015 despite their target of only $3.7 billion.106 In addition, GAVI already receives 76% of its funding from various governments and 18% from the Gates Foundation.107 Hepatitis B vaccinations are therefore far from neglected, and we do not currently recommend donating to such initiatives as it is therefore unlikely that additional donations will have a substantial impact. Likewise, we have not found any other organisations which focus on immunisation which we can currently recommend as both highly cost-effective and sufficiently neglected.108
However, targeting other region-specific causes of liver cancer may also be promising. High rates of liver fluke infection occur in some areas of eastern Asia, especially within the Mekong River Basin in Southeast Asia, where around 40 million people are infected.109110 The worms can infect a host for many years, causing damage to the liver’s bile ducts which can eventually lead to cancer.111 Treatment of liver fluke with Praziquantel can clear the infection and prevent incidence of liver cancer, though people in the area are often quickly reinfected by eating raw fish dishes.112 The Deworm the World Initiative (DtWI) is one charity which administers Praziquantel in Vietnam, where liver fluke are extremely prevalent113 and liver cancer causes 4.81% of all deaths (three times the developing world average).114 However, Vietnam forms only a small proportion of DtWI’s operations (less than 5% of total spending)115 and donations to DtWI, overall, are hence unlikely to cost-effectively reduce liver fluke infection or liver cancer.
Another contributor to liver cancer in the developing world is poor food storage. Parasites can infect staple foods during cultivation, including peanuts, rice and corn.116 In areas where these foods are then stored in warm, high humidity environments, the fungus is able to grow, producing the highly potent aflatoxin. This toxin causes DNA mutations and is associated with both liver and lung cancer.117118 In people with chronic Hep B infection, exposure to aflatoxin increases their chances of liver cancer by 30 times.119120 Improved grain storage and cultivation methods can reduce the amount of the toxin that people consume. With 4.5 billion people currently exposed to aflatoxin, the potential for reducing suffering through changing grain storage practices is enormous. Again, we are not aware of any charities working in this area with sufficient evidence to demonstrate their cost-effectiveness in preventing cancer cases.
Bladder cancer can also potentially be prevented through similar means. Much like liver flukes for liver cancer, infection with Schistosoma haematobium has long been associated with bladder cancer,121 and is recognised as a cause of cancer by the IARC.122123 Studies in the 1970s and 80s noted that bladder cancer was more common in areas in which Schistosoma haematobium infection was common124 and biopsies of tumours showed high incidence of schistosome infection.125126 In one area in South Africa, 53% of those carrying schistosoma haematobium were also found to have developed bladder cancer.127 Across sub-Saharan Africa, Yemen, Sudan, and Egypt, 41-42% of those suffering from bladder cancer also have schistosoma parasites present,128 and hence might be responsible for up to 42% of bladder cancers in this region.
Fortunately, schistosomiasis is easily and cheaply treatable, and two highly effective charities - the Schistosomiasis Control Initiative129 and Deworm the World Initiative130 - can provide treatment for approximately $2 per person per year.131132 Less fortunately, however, schistosomiasis treatment is unlikely to be a cost-effective and efficient method of reducing the incidence of bladder cancer. The annual death toll of bladder cancer in sub-Saharan Africa is only 7,376 (slightly less than Germany alone, which experiences 7,491 each year).133 Given that approximately 42% of cases were due to schistosomiasis, this gives an estimated death toll of approximately 3,100 from bladder cancer in patients who also carry schistosoma parasites. Even supposing, quite conservatively, that schistosomiasis is the direct cause of bladder cancer in all 3,100 patients, this still results in an exceedingly low rate of bladder cancer among schistosomiasis patients. Across sub-Saharan Africa, approximately 120 million people carry the parasite and display symptoms,134 20 million display chronic symptoms,135 and 11.7 million receive treatment each year.136 Even assuming, quite conservatively, that schistosomiasis is the direct cause of bladder cancer in all of those 3,100 patients who die from bladder cancer, only 1 in approximately 38,700 schistosomiasis patients will develop bladder cancer and subsequently die from it. Thus, approximately 38,700 treatments would be required to save one life and, even at $2 per treatment, the cost per life saved is more than $77,000. Admittedly, this figure is not entirely rigorous and almost certainly an underestimate, but it does indicate very strongly that schistosomiasis treatment is not a cost-effective method of reducing the incidence of bladder cancer. In comparison, the Against Malaria Foundation137 prevents a death from malaria for approximately $3,461 and, from above, Project Healthy Children prevents a death specifically from stomach cancer for $19,100 (see Section 5.1).
(Of course, when the more direct benefits of schistosomiasis treatment are considered, the operations of the Schistosomiasis Control Initiative and Deworm the World Initiative are shown to be highly cost-effective. However, here we are restricting our focus to their effect on reducing cancer mortality.)
5.4 Screening, HPV vaccination (cervical cancer)
The WHO and DCP3 also identify methods of reducing deaths from cervical cancer as highly cost-effective, particularly screening and vaccination against Human Papilloma Virus (HPV). However, due to its crowdedness and/or low cost-effectiveness, we do not recommend donations in these area.
For instance, screening and treatment for early cervical lesions have been shown to be cost-effective by both DCP3 and the WHO. In particular, opportunistic screening with an acetic acid test is low-cost and cancerous/precancerous lesions can be removed on the same day.138139
Since high-risk strains of HPV are responsible for up to 98% of cervical cancer cases,140141 HPV screening can also be highly effective in averting deaths from cervical cancer.142 Screens are low-cost and some can be done at home, so women who do not want to come to the clinic or undergo a cervical examination can still be screened.143
Vaccination against HPV strains 16 and 18 (those most commonly associated with cervical cancer) is also highly cost-effective in some areas.144 These vaccinations are included in the DCP3 recommendations, though not the WHO “Best Buys” list. HPV-16 and -18 are responsible for more than 70% of cervical cancers,145 with HPV-16 detected in 57% of cervical cancers and HPV-18 detected in 17%.146 Along with 6 less common strains, these HPV types are responsible for over 90% of cervical cancer cases.147
The HPV vaccine is relatively high-cost and does require two follow-ups, so it may not be cost-effective in all areas.148 However, heavily subsidised vaccines, such as those offered by GAVI alliance, make vaccination much more cost-effective (vaccines at $5 per dose are available to 37 countries in Sub-Saharan Africa).149 The vaccine requires a cold chain, making some areas of sub-Saharan Africa difficult to cover, but it has been estimated that 70% coverage of 9-year old girls for 5 years could avert 670,000 cases of cervical cancer in the region.150
Again, however, we are not aware of any charitable organisations working in this area which are both highly cost-effective and experiencing a sizeable funding gap. Additional donations to the GAVI Alliance, for instance, are unlikely to have a large impact.
5.5 Screening, awareness raising (breast cancer)
Included in the DCP3,151 but not the WHO recommendations, is screening for breast cancer. This prevents patients from going untreated for extended periods of time and thereby from advancing to later-stage cancer, and may be greatly improved by increasing awareness and understanding of the disease. Since presentation with advanced-stage tumour is more common in low/middle income countries,152 examination by medical professionals and education in breast self-awareness may decrease death rates, as treatment earlier in the disease course is far easier and has a higher success rate.153
A case study in Malaysia found that incidence of patients presenting at late stage breast cancer decreased from 77% to 37% after a country-wide drive to increase awareness. As part of the drive, nurses began to visit rural areas to give talks, demonstrate breast awareness and perform examinations.154
We are not aware of any charitable organisations working in this area which are both highly cost-effective and experiencing a sizeable funding gap. However, Development Media International (DMI) is one charity which raises awareness of various health issues in developing countries and which is supported by rigorous evidence and independent evaluations.155 DMI targets its awareness campaigns at the most tractable, neglected and high-impact areas and health practices. Based on these priorities, DMI has not focussed on breast cancer awareness thus far but instead prioritised those health practices which have greater potential to save and improve lives. This might indicate: a) that breast cancer awareness simply is not as high-impact or tractable as other interventions in DCP3 and recommended by the WHO; and b) that a lack of funding has not permitted DMI or other charities in this area to pick the ‘low-hanging fruit’ of higher-impact awareness initiatives and move on to breast cancer and others.
6. Treatment
Cancer costs in developed nations are generally quite high. In the United States, for instance, the mean cost of treatment of patients in their initial year after diagnosis is above US$50,000 in most categories of cancer, and exceeds US$100,000 for some categories.156 Including ongoing costs in subsequent years of treatment, the cost of cancer treatment in the United States is exceedingly high - in comparison, donations to the the Against Malaria Foundation (one of the top charities recommended by Giving What We Can) prevent deaths of children under the age of 5 in sub-Saharan Africa for approximately $3,461 per person.157 The situation is similar in the United Kingdom (with an average annual treatment cost of £30,000 per person, predominantly borne by the government)158 and elsewhere, with the additional consideration that government initiatives such as the National Health Service, or private insurers, often cover the costs of treatment. Indeed, funding has even been allocated for those cancer treatments which fail to meet cost-effectiveness standards - £416 million per year in the UK.159 The relatively high per-capita income in such developed nations160 also makes it plausible that many patients would simply pay for their own treatment if no other funding were available. Thus, the impact of donations towards cancer treatment in such nations is unlikely to have any sizeable impact as, not only is the cost of treatment extremely high but, patients are likely to be treated with or without further donations. Hence, it is neither cost-effective nor neglected.
In developing nations, however, the situation is quite different. DCP3 does identify cancer treatment in the developing world among its listed priorities.161 It offers an “Essentials Cancer Intervention Package” designed to reduce deaths from cancer, both through treatment and through prevention, and which is tailored to the wealth and infrastructure of the country in question. In particular, DCP3 highlights the cost-effectiveness of treating some childhood cancers. The very high cure rates seen in some childhood cancers in HICs are often dependant on intensive supportive care which is not available in LICs162. However, some studies have shown less intensive treatments of certain cancers to be highly cost-effective, with a combination drug treatment of Burkitt’s Lymphoma, for instance, costing less than $1000 per successful treatment.163164165166 One study even showed that a 28-day treatment cycle, costing less than $50 per patient to perform, had a 50% survival rate167 - hence suggesting that a life might be saved for less than $100. Unfortunately, however, we are not aware of any underfunded charitable organisations which focus on providing highly cost-effective treatments such as this.
One strategy which may facilitate improved and broader treatment of childhood cancers in developing nations is the use of twinning programs. That is, the linking of hospitals in low income countries (LICs) with specialist hospitals in high income countries (HICs) to allow expertise to be shared and thereby improve treatment and survival rates.168 DCP3 also notes that this may have positive flow-on effects - the success seen in childhood cancer can act as a strong motivator to encourage governments to pursue cancer treatment programs and give early stage patients the hope required to seek help as soon as they discover symptoms of disease.
Twinning programs are one of several interventions performed by World Child Cancer,169 an international cancer treatment charity which does appear promising and which also treats Burkitt’s Lymphoma, however they admit that they do not focus on the most cost-effective treatments and programs. Even though some of their interventions such as twinning programs may be highly effective, we do not believe that a large portion of donations will be spent on such interventions and, therefore, that donating to World Child Cancer is not a highly cost-effective method of having an impact. In addition, we are not aware of any other underfunded charities carrying out treatment interventions which have a sufficient focus on the most cost-effective treatments.
- *[^fn-91]: We are estimating this proportion from the rates of vitamin A deficiency among children of preschool age which, although different from the rate population-wide, does give a rough indication of what proportion of the population are not receiving adequate levels of vitamin A and are therefore well-placed to benefit from fortification.